Victor Rao MBBS, DMRD, RDMS (APCA)
A Brief History of Joint Injection
Joint injections have been performed since the end of the 19th century. Clinicians would inject anti-inflammatory or disinfecting agents into the joint spaces to provide pain relief to patients. After cortisone became commercially available by Merck in 1929, medical professionals began injecting the steroid into the joint spaces instead. During the 1950s, it became the pain-relieving treatment of choice. To this day, clinicians around the world inject joint spaces with cortisone and other therapeutic agents.
The procedure was initially performed using the surface landmark technique and was essentially a blind technique since ultrasound or other imaging forms were unavailable during those times. The landmark method required a thorough knowledge of anatomy and a significant amount of practice and experience over the years to achieve proficiency. Even with considerable experience, there was still the potential risk of making an error sometimes due to variances in the patient’s anatomy or other factors such as the patient’s body habitus or anatomical deformity.
Injections Using POCUS Guidance
With the introduction of Point-of-Care Ultrasound (POCUS), the procedure has become easier to learn and master. Now, every healthcare provider who wishes can access an ultrasound device and perform joint injections using ultrasound guidance. Performing this procedure with POCUS ensures the clinician administers the corticosteroid and/or anesthetic agent at the correct location with reduced risk of injuring surrounding structures or delivering the medication in a suboptimal site.
POCUS has also shortened the learning curve, and now any provider with a good baseline knowledge of the relevant anatomy and adequate hands-on training can perform these procedures with a high degree of accuracy and increased confidence.
Nerve blocks have been performed since the 1950s. It is the next popular application that uses ultrasound guidance to achieve optimal regional anesthesia. The goal is to block the pain signal from nerve receptors in a specific region of the body, which is achieved by injecting an anesthetic agent around that specific nerve to provide local anesthesia.
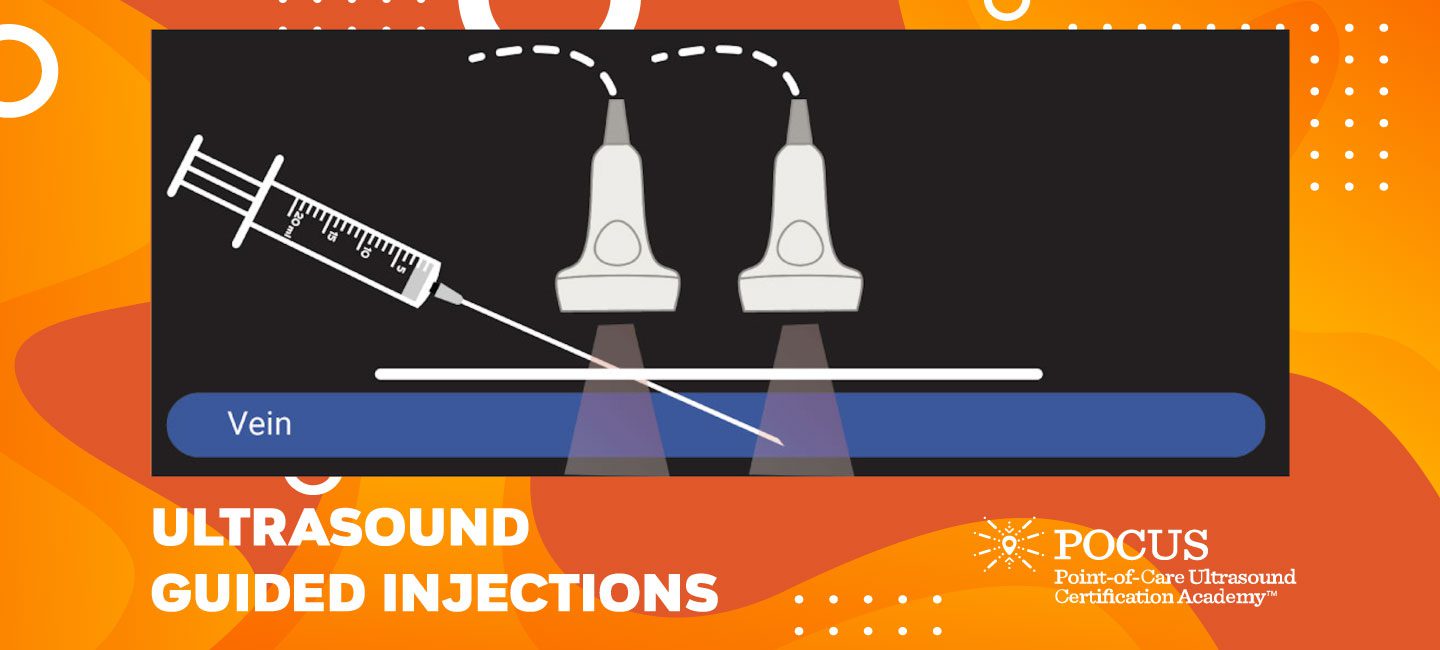
Both the above procedures have a steep learning curve if performed using surface landmarks only. Learning to perform these procedures using ultrasound to image the targeted region has flattened the learning curve. POCUS has allowed users performing the procedure to observe the needle as it advances through the tissues and provides real-time viewing of the medication being delivered to the correct site.
The patient’s written consent must be obtained before conducting the procedure. It is also essential to have a list of medications the patient is on to avoid prolonged bleeding after the procedure. Inform diabetic patients that they may experience a temporary rise in blood sugar levels for two to three days after the steroid injection.
How To Perform The Procedure
The transducer of choice would be a high-frequency linear transducer unless the target is deeper, in which case a low-frequency curvilinear transducer may work better. Disinfect the area of access following recommended guidelines. It is always a good idea to perform a quick pre-scan to familiarize yourself with the patient’s anatomy and any potential risks that could be encountered during the procedure. Be sure to determine adequate needle length before inserting the needle.
There are few approaches to performing injections using ultrasound guidance. The best method is the dynamic approach in which the clinician is performing a real-time ultrasound scan as the needle is inserted and advanced into the tissue. The recommendation is to hold the syringe in the dominant hand. When the transducer is aligned correctly, this in-plane method allows the provider to visualize the shaft of the needle and its tip.
The plane of the needle must be aligned with the mid-longitudinal plane of the transducer to image it. Even if you are off by 1mm, the needle will not be visible on ultrasound. The short axis view is much easier because you will always see the needle shaft or tip. The challenge will be to follow the needle tip. This method is useful for injecting superficial joints. Some newer devices offer simultaneous Bi-Plane imaging, which is the best method for observing the needle in real-time in both the transverse and longitudinal planes.
In conclusion, all joint injections or nerve blocks should be performed using ultrasound guidance. Some medical professionals who may already perform nerve blocks and joint injections using the landmark technique will find it an easy transition. This is one of the many POCUS skills that most clinicians have readily adopted.
Want to start your POCUS journey today? Check out our many certificate and certification programs.





















