By Victor V Rao MBBS, DMRD, RDMS
Introduction
Abdominal aortic aneurysm (AAA) is defined as a focal dilatation of a segment of the abdominal aorta with an outer wall to outer wall diameter of 3.0 cm or more. The normal abdominal aorta diameter in an average healthy adult is approximately 2.0 cm. When AAA diameter is 5.5 cm or more, it is considered high risk for rupture and thus an elective repair is recommended to reinforce the aneurysm wall to prevent rupture or leak of the AAA. Approximately 200,000 individuals are diagnosed with AAA in the United States every year. Abdominal ultrasound is the screening modality of choice for AAA because of low cost, no ionizing radiation, a very high specificity of 100% and a high sensitivity of 95-100%. These numbers vary slightly in different studies, but we can all agree that ultrasound is an excellent and reliable low-cost imaging modality to diagnose AAA.
Common Signs and Symptoms
Most abdominal aortic aneurysms are asymptomatic with no obvious physical signs and could be found accidentally while performing a physical examination, an abdominal ultrasound scan or some other abdominal imaging study such as a CT scan or an MRI performed for other indications. Some studies suggest that the physical exam has low sensitivity for detecting AAA. The sensitivity of abdominal palpation for detecting a possible AAA varies from 61% to 82% depending on the size of the AAA. The higher sensitivity of 82% was reported in AAAs measuring 5.0 cm or higher. However, if it a large or gigantic AAA and the patient is thin, physical examination should be able to diagnose the condition or raise suspicion about the possibility of a AAA in 100% of cases. Body habitus, bowel gas and other factors may pose challenges when performing an ultrasound examination. Let us look at an image from an article (see references also) which reported a patient with an unusually large AAA measuring 25.0 cm in diameter. This case could be diagnosed as the patient walked into the clinic by simple observation alone. But these are very rare cases. However, it is good to be aware that AAAs can become extremely large without rupturing in rare cases.

Figure 1. Patient with a giant abdominal aortic aneurysm presented with a palpable pulsatile intraabdominal mass. Image courtesy of Dainis Krievins, MD, PhD et. al.
The following symptoms may also suggest the possibility of ruptured AAA as a differential diagnosis. Keep in mind these symptoms are not specific to AAA.
- Sudden pain in the back or abdomen.
- Dizziness.
- Nausea/vomiting.
- Clinical shock with increased heart rate.
- Pain radiating to the buttocks, groin, or legs.
Role of Ultrasound as a Diagnostic Tool
B-mode/2D ultrasound is very helpful in assessing the abdominal aorta for an abdominal aortic aneurysm. Scan the entire length of the abdominal aorta as it enters the abdominal cavity through the aortic hiatus in the diaphragm all the way to the level of bifurcation of the lower abdominal aorta into the left and right common iliac arteries as shown in Figure 2.
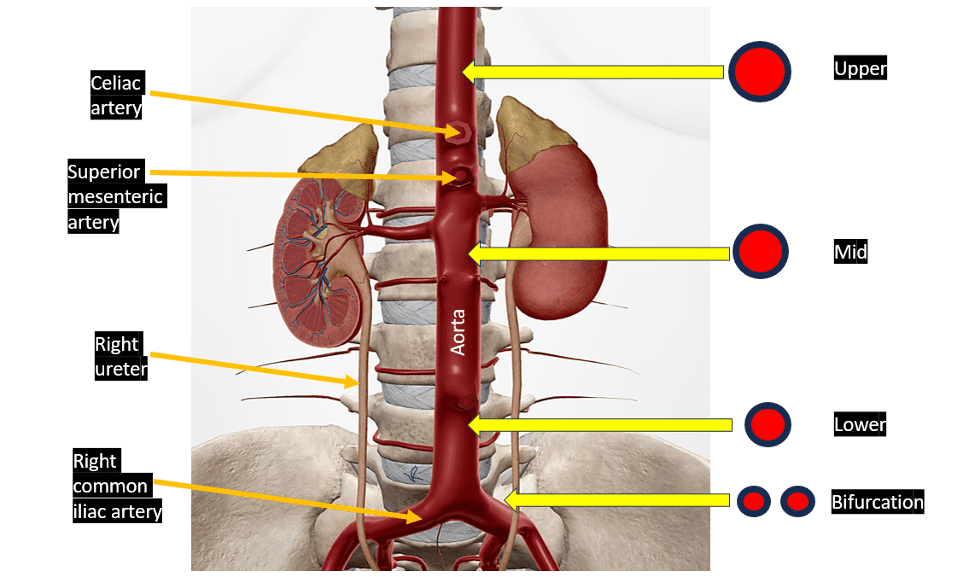
Figure 2. Diagrammatic representation of the abdominal aorta. Some vessels and anatomical structures have been removed to show the abdominal aorta clearly. The transverse views recommended should be obtained in the upper, mid, lower abdominal aorta as shown on the right of the image. One view of the bifurcation should also be captured as shown on the right side of the figure. In addition, capture and save mid-longitudinal views of the abdominal aorta at the 3 levels. If a dilatation or aortic aneurysm is seen, additional paired views of the aneurysm segment should be captured. Measurement of the aorta should be done from outer wall to outer wall.
How to Measure Abdominal Aorta Diameter using B-mode ultrasound
Mid-longitudinal Views
Obtain mid longitudinal views in the upper, mid, and lower abdominal aorta. Measure from outer wall to outer wall at the level where the abdominal aorta diameter seems to be the widest.
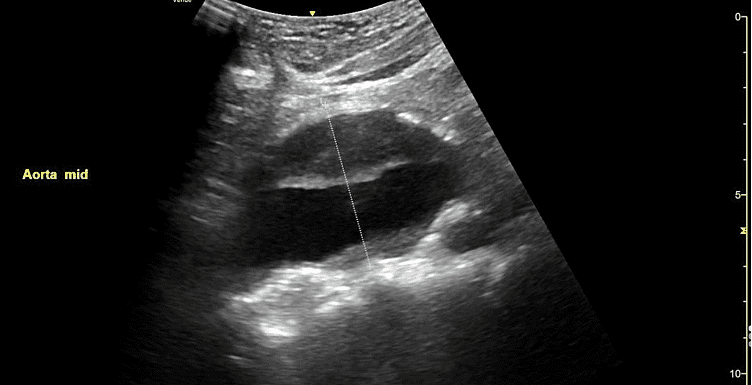
Figure 3. Fusiform abdominal aortic aneurysm. Observe that the thrombus has been included in the measurement. The measurement should be done perpendicular to the posterior wall of the aorta.
Transverse Views
Obtain the transverse views of the abdominal aorta at the upper, mid, and lower levels. Measure from outer wall to outer wall (antero-posterior and side by side). See Figure 4.
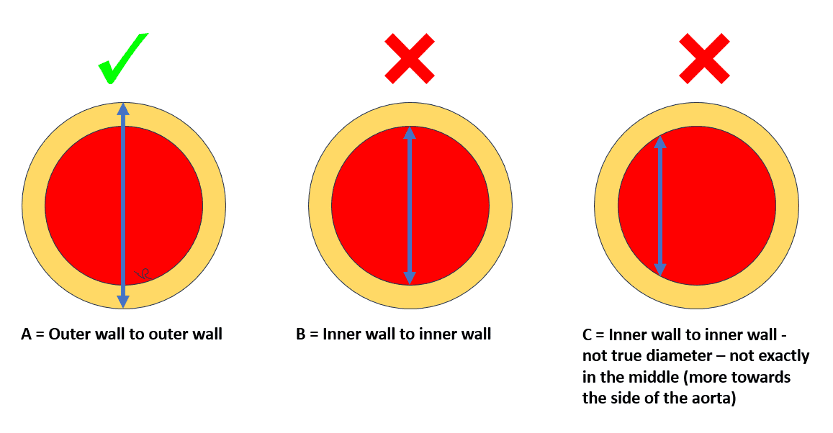
Figure 4. A represents measurement of aorta using the correct technique (outer wall to outer wall and in the middle of the aorta). B represents measurement from inner wall to inner wall which is incorrect. C shows measurement from the side and inner wall to inner wall which is incorrect.
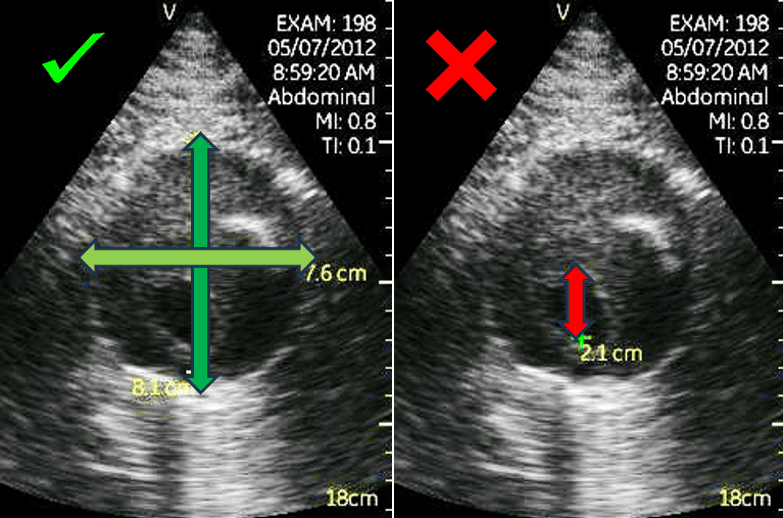
Figure 5. The image on the left shows the correct method to measure an AAA diameter. The image on the right shows the incorrect method to measure. This patient was previously incorrectly diagnosed as not having an AAA by another imaging team. They had incorrectly measured only the residual lumen of 2.1 cm. After correct measurement technique was applied during a follow up ultrasound the maximum abdominal aortic aneurysm diameter was reported as 8.1 cm. The patient was referred immediately to a vascular surgeon for elective repair and did well after the endovascular aneurysm repair (EVAR) procedure. Image courtesy of Dr. Steven Burns MD
Final Thoughts
It is important to measure the abdominal aorta diameter from outer wall to outer wall because the patient management depends on the maximum diameter of the aneurysm. If an aneurysm is present, then place calipers at the widest points. If there is a plaque, or a thrombus present within the aneurysm you must include those within the calipers if they happen to be in the plane of the widest region of the aneurysm. Do note that the upper abdominal aorta is cephalad to the level of the celiac artery. If an aneurysm is diagnosed, it is important to make the patient aware of the diagnosis and the importance of serial follow up ultrasound exams as an aortic aneurysm tends to increase in diameter with time. Elective repair of an aortic aneurysm is indicated if the aneurysm maximum diameter is 5.5 cm or more or the aneurysm is observed to be increasing in diameter by 1.0 cm or more per year on serial follow up ultrasound examinations. Your institution may have their own specific protocol that they follow, and it may vary slightly. The goal is to consider elective repair before the AAA ruptures because it is associated with sudden death in some instances or increased morbidity and mortality with poor outcome. POCUS users can make a huge impact by identifying this potentially life-threatening condition and advising the patient accordingly. It is important to remember that ultrasound may not be sensitive enough to diagnose a leaking or ruptured AAA because most AAAs leak into the retroperitoneal space and that may be difficult to diagnose on ultrasound. If the patient is hemodynamically unstable and all you see is a AAA, then it would be safe to consider other imaging modalities such as CT scan and assume that the patient has a ruptured AAA unless ruled out by CT scan. Consider performing the RUSH protocol to rule out other potential causes of shock and hypotension.
References
- https://www.pocus101.com/aorta-ultrasound-made-easy-step-by-step-guide/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3076160/
- https://www.aafp.org/pubs/afp/issues/2020/0515/od1.html
- https://www.pocus.org/resources/screening-of-abdominal-aortic-aneurysm-aaa-using-point-of-care-ultrasound/
- https://www.youtube.com/watch?v=qUpXJBoAoWI
- https://www.jvascsurg.org/article/S0741-5214(14)01731-5/pdf
- https://pubmed.ncbi.nlm.nih.gov/10737283/
- https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/485262
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7227275/





















