Written by James Day, RDCS
We’ll walk through how to get the best possible on-axis, Apical 4 chamber view so that you can evaluate wall motion and gain a sense of left ventricular (LV) function.
The key to maximizing ultrasound imaging is patient body manipulation and breaths. Before you touch any knob, get your patient in the best possible position to optimize your images. Have your patient roll into the left lateral decubitus position (assuming they have no spine issues). Most won’t understand this term, so I tell them to roll over like they are taking a nap. Have them stretch their left arm under a pillow, with their right arm on their side.
This position allows the heart to “fall” closer to the chest wall. The outstretched arm will spread your patient’s ribs somewhat, allowing a larger window between the intercostal spaces for your phased array transducer with its small footprint to get between highly reflective bones.
If you have a “lung curtain” that obscures your Apical 4C view, have your patient exhale and then hold their breath (you can also grab recording clips when the lung retracts back). If you are right-handed, move your transducer to just under the patient’s left pectoral muscle or left breast and drop the tail down so that the transducer is tilted cephalad at about a 60-degree angle. Typically you will also have to swing the tail out laterally a few degrees, so you are facing back toward the midline slightly.
Now to assist you in finding the apex, have your fingers overhang your phased array transducer so that you can also conduct a physical exam and find the point of maximal impulse (PMI) with your fingertips. A move I often do next is to take your patient’s right shoulder and pull it gently back. This move rolls them over a small amount allowing you to get more lateral and open the intercostal spaces further. It also puts you on a nice angle, so the beam “slices” the Apical 4C view perfectly in half. Imagine cutting a bell pepper from stem to bottom, exposing all four chambers equally.
Now let’s look at our screen. I want to see the LV apex tucked right into the “tent” of the sector. Do not cut off your LV — If you are still off-axis, 99% of the time, you need to go more laterally on your patient.
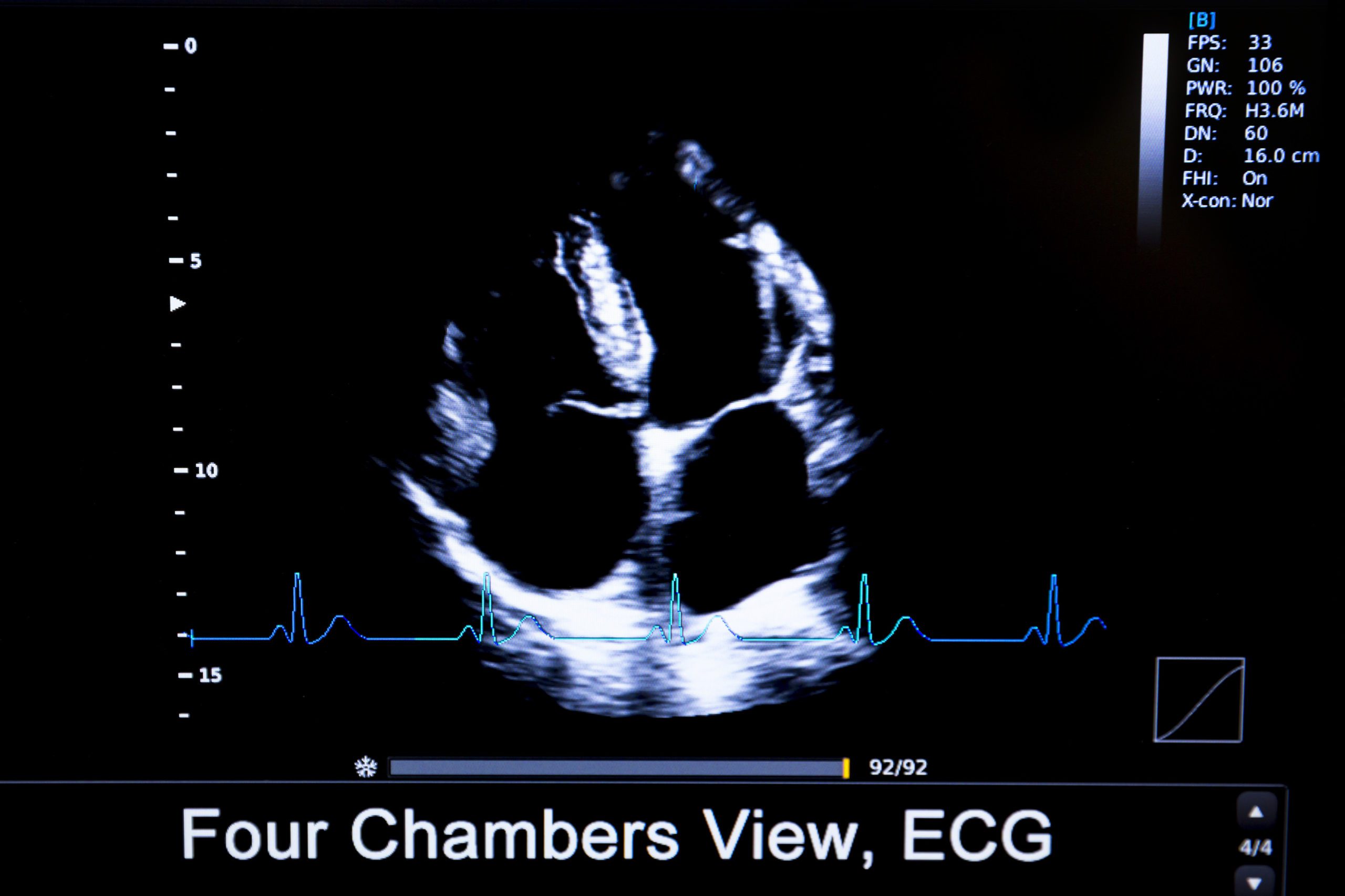
The LV should be 7cm in length and look like a football, a nicely shaped oval. If it appears global or looks like a softball, then you are foreshortening the apex of the LV — merely drop-down (caudal) an intercostal space. A technically good-quality apical view will have the interventricular septum running straight down the middle of the screen. You should be able to see both the mitral and tricuspid valves clearly. Ideally, you’ll also see the LV and right ventricular (RV) free walls in your view.
Note that the inter-ventricular and inter-atrial septum are centered on the screen and oriented vertically. The MV and TV are both visible, suggesting you are getting a slice through the true center of the heart. Signal dropout in the basal portion of the interatrial septum is common and does not represent an ASD.
Now let’s look at the LV. I always recommend increasing the depth as zoom only makes a bad image bigger. Now place the LV perfectly inside of the entire sector. Note the endocardial border architecture. See all the trabeculations. Is the endocardium squeezing? Are the opposing walls almost “kissing”? If so, most likely, you have a normal ejection fraction and good LV systolic function.
We are merely “eyeballing” LV function here. We will not be using a Simpson or Modified Simpson to calculate an equation. Leave that to the sonographers and the follow-up exam. Your job is a quick evaluation to make a clinical patient management decision. Is the LV function at rest, normal or mild, moderate or severe?
Take note of the tiny thread in the upper LV apex. That is the pseudo tendon, sometimes mistaken for a linear thrombus. Look over into the RV. The moderator band can be seen here. Recall this is a normal muscular band of tissue that extends in a horizontal orientation across the RV.
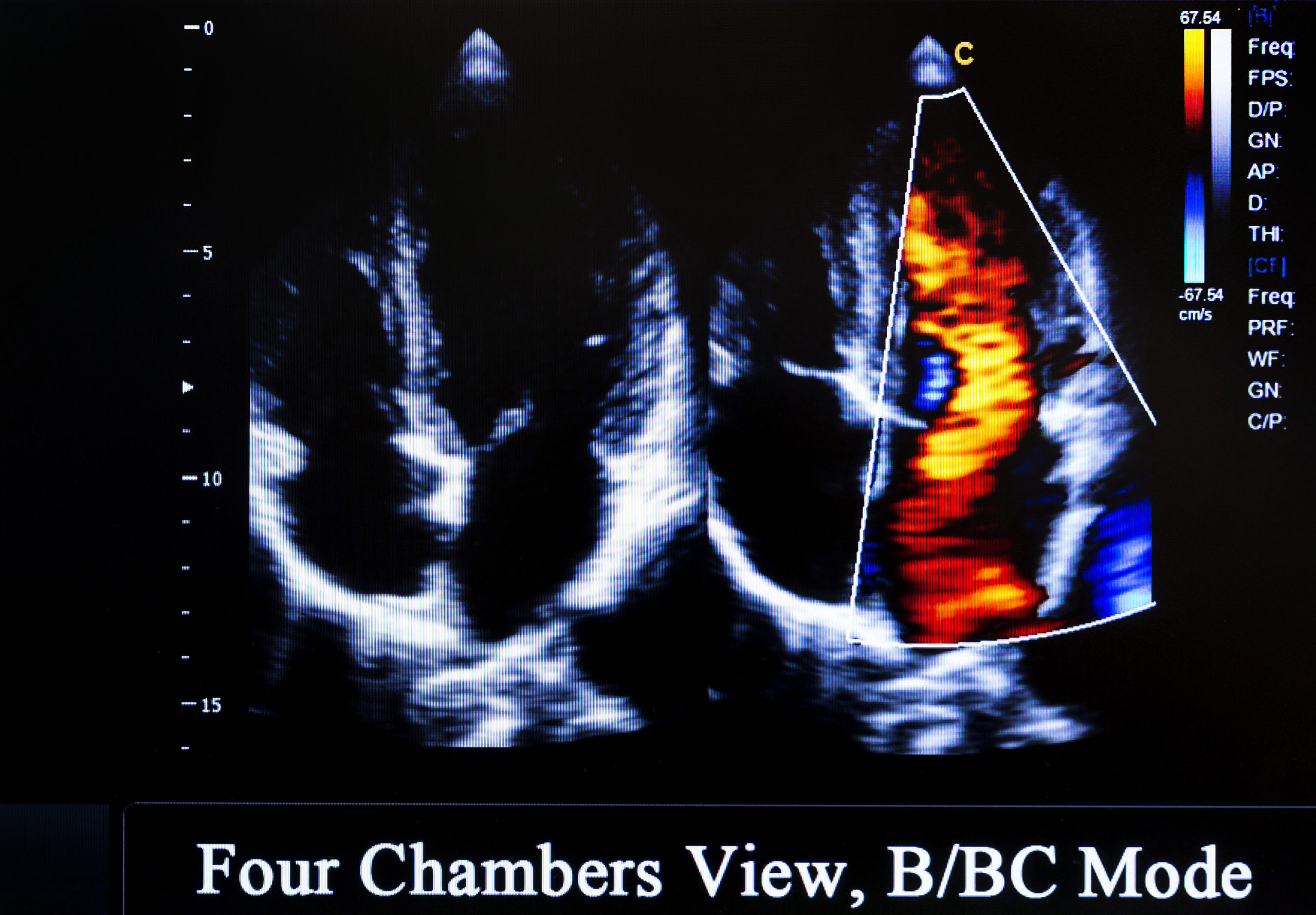
After getting a good quality Apical 4 chamber, tilt the transducer upwards slightly to visualize the aorta (the 5th “chamber”), which is more anterior. Note the left ventricular outflow tract (LVOT) and the aortic valves. Are they highly echogenic? Do they appear pliable, or are they like rusted hinges from calcification?
Ca+ accumulation leads to varying degrees of aortic stenosis. Close off the 5th chamber with a transducer tilt and evaluate the MV and TV. Are they pliable and moving with ease in a rhythm? Do you see any vegetations or thrombus?
Look closely at the TV, are there small “seaweed” like fuzz on the valves. It’s hard to see, but you can catch it at times. Is the mitral valve doing its LV inflow and atrial kick “dance”? Do the values look stenotic? What about the point of valvular insertion?
I hope you enjoyed this basic Apical 4 Chamber tutorial. In my experience the most challenging of all the POCUS exams are cardiac (staying on-axis), MSK ( for the anatomy), and appendix (hard to find).
Looking for additional inspiration? Sign up for our POCUS Post™ newsletter to receive monthly tips and ideas.





















