Victor V Rao MBBS, DMRD, RDMS- Abdomen, Ob/Gyn (APCA)
Introduction
Deep vein thrombosis (DVT) is a medical condition in which a blood clot develops in a deep vein, usually in the leg and/or thigh. It can also form in the pelvic veins or upper extremities. DVT can be life-threatening if the blood clot breaks loose. It can travel to the lung, becoming potentially fatal if it is large enough to obstruct blood flow to the left and right lungs. This happens when a large clot gets obstructed in the pulmonary artery, where it divides into the left and right pulmonary arteries. This type of embolus is known as a saddle embolus and can result in sudden death.
DVT is often underdiagnosed and can affect individuals of any age group. It is a preventable medical condition. Early diagnosis and treatment can prevent morbidity and mortality in patients. According to the Centers for Disease Control and Prevention, up to 900,000 patients are affected by this condition resulting in 60,000 to 100,000 deaths in the U.S. annually. Unfortunately, 10-30% of the individuals will die within a month of diagnosis.
There are a few alarming insights about DVT. In 25% of individuals with the condition, sudden death may be the first symptom noted in those with a hemodynamically significant pulmonary embolism (PE). Up to 33% of individuals with DVT will have a recurrence within 10 years. Even though some patients may be successfully treated, 33% to 50% of those may still have swelling, discoloration, scaling, ulcers, and pain in the affected limb.
Common Signs and Symptoms
A small DVT or PE could also be asymptomatic. Some common signs and symptoms of DVT may include the following.
- Difficulty breathing (dyspnea)
- Tachycardia
- Chest pain
- Hemoptysis
- Hypotension
- Lightheadedness
- Fainting
Ultrasound as a Diagnostic Tool
Ultrasound is an excellent diagnostic tool used to diagnose DVT. It is non-invasive and has become relatively inexpensive and more accessible with the introduction of multiple point-of-care ultrasound (POCUS) devices in the market. These devices use high-frequency ultrasound waves to create images of the blood vessels and surrounding tissue. During an ultrasound examination for DVT assessment, acoustic coupling gel is applied to the skin, and an ultrasound transducer is used to identify the deep veins of the lower extremity.
The point-of-care DVT assessment is an important and seamless POCUS skill to learn. Every clinician should be able to learn to effectively diagnose a simple case of DVT by undergoing a short training course which must include hands-on training on standardized patients and actual patients with DVT. It is recommended to perform a 3-zone compression test using B-mode ultrasound. Always examine both lower extremities. Even though the patient may present with redness and swelling in the affected limb, there have been situations where the DVT was found on the opposite lower extremity.
Ultrasound can help diagnose clots in the deep veins, including those in the leg, thigh, and pelvis. It can also be used to evaluate blood flow using color Doppler and spectral Doppler. The method, however, has some limitations. It is not always 100% accurate. In some cases, the images produced by ultrasound may be difficult to interpret, especially if the clot is in a challenging location with poor visualization of the deep vein.
Overall, DVT assessment using POCUS is destined to make a significant difference in the mortality and morbidity rates associated with DVT through early detection and treatment. Be aware that the blood clot may or may not be visible on B-mode ultrasound. The B-mode compression test is the gold standard and should be adopted by all involved in patient care.
Features of Blood Clot on B-mode ultrasound
B-mode ultrasound is recommended while scanning for DVT assessment. However, other modes, such as color and spectral Doppler, may also be done in addition to the B-mode compression test. Healthcare providers generally ask, “Can we always see a blood clot using B-mode ultrasound?” The answer is “No .” Therefore, we cannot simply rely on the B-mode image and must perform the compression test accurately. Also, be aware that sometimes a blood clot can be anechoic (black) and may appear just like liquid blood. In some cases, there may be an echogenic artifact that may seem like a clot in the lumen of the deep vein.
An acute DVT may appear hypoechoic, anechoic, or even isoechoic with the surrounding unclotted blood. That is why the compression test is essential. While performing the compression test, interrogate the vein in the middle of the images, as the vein may move to the side during compression. Compression must always be performed in the transverse view. A subacute DV may have a variable appearance. A chronic DVT tends to be more hyperechoic/echogenic in appearance. It is important to note that a clot may be partially compressible. So, this procedure heavily depends upon the individual performing the compression test.
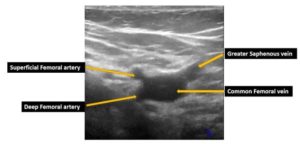 Figure 1. A transverse view obtained at the right saphenofemoral junction before the compression test. This image was acquired with the probe marker pointing toward the patient’s right side.
Figure 1. A transverse view obtained at the right saphenofemoral junction before the compression test. This image was acquired with the probe marker pointing toward the patient’s right side.
Moderate pressure is applied with the transducer. In a normal vein with no blood clot present, the anterior and posterior walls of the vein should touch each other with no residual lumen. If the walls do not touch, there is either a blood clot within the lumen of the vein or the pressure applied is inadequate. This can be a real challenge if the clot is anechoic or hypoechoic. Always consider applying counter traction when needed by placing your hand precisely on the opposite side of the limb in line with the transducer. Sometimes you may be able to see a hypoechoic or hyperechoic clot with the lumen of the vein. In either case, compress cautiously to prevent breaking the clot and causing a pulmonary embolism (PE).
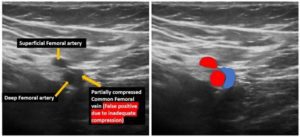 Figure 2. Transverse view at the saphenofemoral junction. Observe that the common femoral vein was not fully compressed. This patient did not have a DVT. This was a false positive. It is important to note that this procedure is user dependent. If the correct technique is not used, it may lead to a false positive result.
Figure 2. Transverse view at the saphenofemoral junction. Observe that the common femoral vein was not fully compressed. This patient did not have a DVT. This was a false positive. It is important to note that this procedure is user dependent. If the correct technique is not used, it may lead to a false positive result.
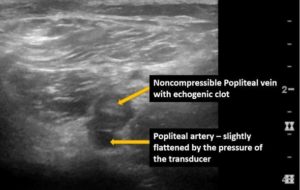 Figure 3. A transverse view obtained at the level of the popliteal crease. Observe the non-compressible popliteal vein. The blood clot/thrombus is visible on B-mode in this case. Keep in mind that the thrombus may be anechoic also. So, the gold standard is the compression test using B-mode ultrasound.
Figure 3. A transverse view obtained at the level of the popliteal crease. Observe the non-compressible popliteal vein. The blood clot/thrombus is visible on B-mode in this case. Keep in mind that the thrombus may be anechoic also. So, the gold standard is the compression test using B-mode ultrasound.
Final Thoughts
In conclusion, DVT 3-zone compression test is an excellent tool available for clinicians worldwide. Providers will want to perform the test cautiously and feel confident about the diagnosis. If in doubt, send the patient to the vascular lab for a full protocol DVT assessment.
The 3-zone DVT assessment is also paired with a D-dimer test. If the D-dimer is negative, then DVT is ruled out. Sometimes D-dimer may be positive. It could also be a false positive or indicative of a DVT. When this occurs, as per your facility protocol, we want to assess the patient for DVT again after one week or sooner. If there is access to a vascular laboratory, send the patient for a full protocol DVT assessment of both lower limbs.
Four valuable references are below to help you master the POCUS DVT assessment.
References
Ahn, J., Dinh, V., Deschamps, J., Genobaga, S., Lang, A., Lee, V., Krause, R., Tooma, D., White, S. DVT ultrasound made easy: Step-by-step guide. POCUS 101. Retrieve from https://www.pocus101.com/dvt-ultrasound-made-easy-step-by-step-guide/
Arfaras, A. M., Balasubramanian, P., Barrera, C. A., Failliace, R. T., Galen, B., Gulani, P., Napolitano, M., Nauka, P., Ntaios, G., Palaiodimos, L., Varrias, D., Zamora, C., Zavras, P. The use of point-of-care ultrasound (POCUS) in the diagnosis of deep vein thrombosis. Journal of Clinical Medicine 2001, 10(17), 3902. Retrieved from https://www.mdpi.com/2077-0383/10/17/3903
Deep vein thrombosis ultrasound image gallery. POCUS 101. Retrieved from https://www.pocus101.com/deep-vein-thrombosis-ultrasound-image-gallery/
Gornik, H., Sharma, A. M. Duplex ultrasound in the diagnosis of lower-extremity deep venous thrombosis. Circulation 2014, 129:917–921. Retrieved from https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.113.002966




















