Victor Rao MBBS, DMRD, RDMS (APCA)
Anatomy
The inferior vena cava (IVC) is a large, thin-walled, retroperitoneal blood vessel formed by the confluence of the left and right common iliac veins. It carries the deoxygenated blood from the lower body and lower extremities to the right atrium. Before it drains into the right atrium, it runs a short course through the liver and collects blood from the hepatic veins. It also acts as a venous capacitance reservoir. The IVC typically runs on the right side of the spine. The image below shows it (the large blue vessel) lying next to the abdominal aorta (Figure 1). Rarely, there could be anatomical variants such as left-sided IVC and IVC duplication.
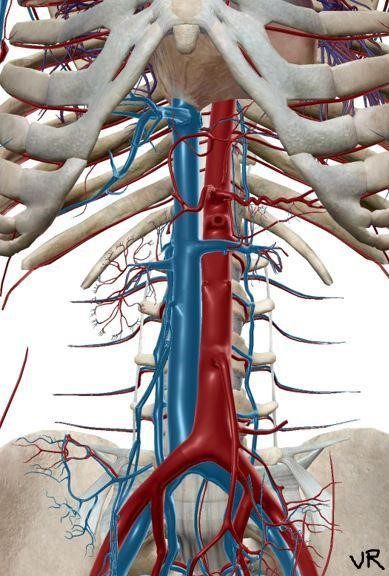
Figure 1. IVC with draining veins is shown in blue. Observe how the IVC drains straight into the right atrium of the heart.
Common Indications
Some common indications for IVC assessment are:
- Determine volume status
- Determine approximate central venous pressure (CVP)
- Determine fluid therapy responsiveness in management of shock
- Determine possible cause of shock
- Monitor response to therapy
- Determine collapsed or plethoric IVC
- Part of VExUS protocol
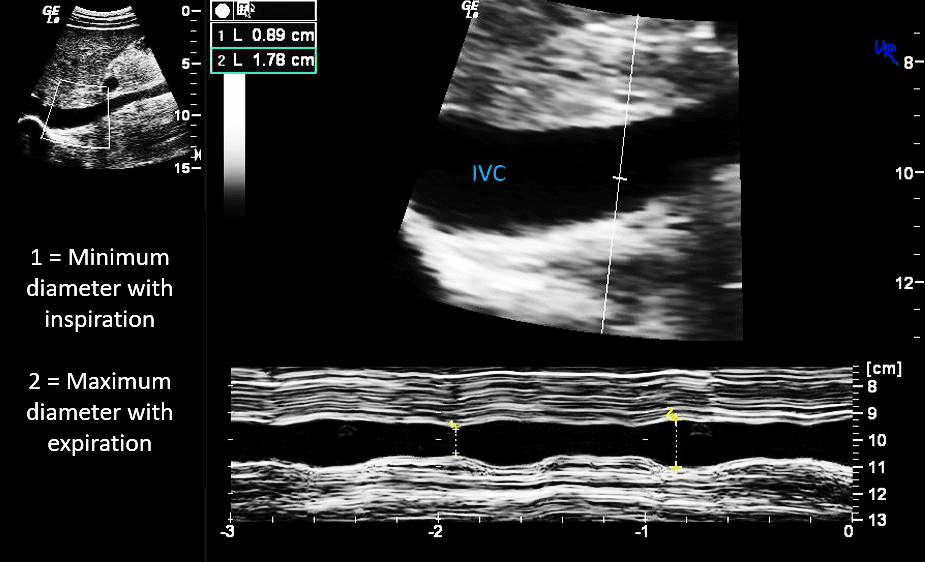
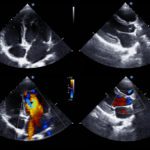
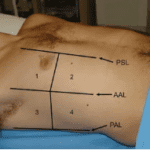
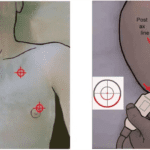
Figure 2. Documenting IVC diameter variability with respiration using B-mode and M-mode.
IVC Diameter and Variability with Respiration – What the numbers mean?
The table below shows the relationship between IVC diameter, respiratory variation, and approximate CVP range.
| IVC diameter (cm) | Respiratory variation | CVP (cm H20) |
| <1.5 | Total collapse | 0-5 |
| 1.5 – 2.5 | >50% | 6-10 |
| 1.5 – 2.5 | <50% | 11-15 |
| >2.5 | <50% | 16-20 |
| >2.5 | No change | >20 |
Measuring and correlating IVC diameter, respiratory variation, and CVP to direct fluid therapy may be controversial at times. However, in most clinical situations, it is of value, such as cases where there is very small or collapsed IVC or large plethoric IVC. The exception to this rule occurs in some challenging clinical scenarios, for example, when the patient is on a mechanical ventilator.
Pitfalls
Some very well-trained and conditioned elite athletes may have a normal physiologically distended IVC due to increased venous reserves. Some examples of pathophysiological IVC dilatation may be cardiac tamponade, pneumothorax, hemodynamically significant pulmonary embolism (PE), some cases of myocardial infarction, and decompensated heart failure. IVC may be small or collapsed in severe dehydration, significant blood loss due to bleeding, and sepsis. In these conditions, the IVC diameter may not be an accurate indicator of volume status.
Implications
Inaccurate determination of volume status may lead to the administration of unnecessary diuretics or reduced fluids. On the other hand, it could also lead to excessive fluid administration or delay of vasopressors.
Mitigation
An inaccurate interpretation of the volume status can be avoided by being aware of the limitations of just looking at the IVC diameter in some clinical situations. For example, you could easily scan both lung fields to look for evidence of pulmonary congestion (B-lines). However, it is highly recommended to consider using the venous excess ultrasound (VExUS) grading system in patients with renal failure, septic shock, and congestive heart failure. Always compare the hemodynamic data with the complete clinical picture and other lab values.
Since the vascular system is all connected, it makes more sense to evaluate hemodynamic flow parameters in the hepatic, portal, and intrarenal veins, as well as the IVC, to gain a more accurate picture. The VExUS score will help determine the grade (Grade 0-3) of venous congestion to manage fluid therapy accurately.
Ready to dive deeper in your knowledge of POCUS? Visit our individual clinical certificate page to check out the many opportunities available.