By Victor V Rao MBBS, DMRD, RDMS
Chest imaging plays an important role in diagnosing and monitoring lung pathologies. While chest X-rays have long been the standard imaging modality since their discovery in 1895, lung ultrasound is emerging as a great alternative in many clinical scenarios specifically in Point-of-Care applications in recent years. We will briefly review and compare these two imaging modalities and explore the strengths and limitations of each modality in three common lung or chest pathologies (See Table 1).
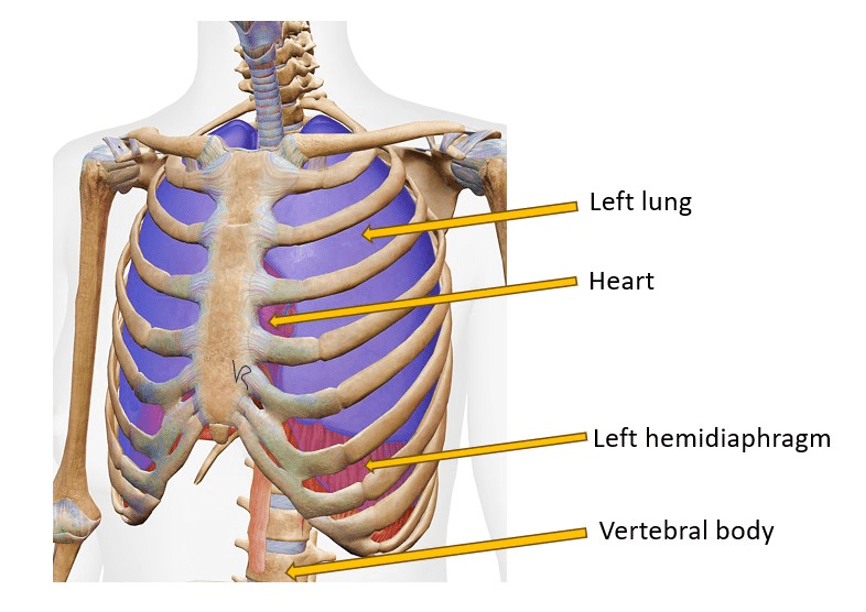
Figure 1. Chest oblique view with superficial skin layer, subcutaneous tissue, muscles and parietal pleura removed (diagrammatic) to show structures inside the chest cavity.
Chest X-ray
Chest X-rays have been the go-to imaging modality for lung and chest pathology assessment for decades. They provide a broad overview of the chest, including the lungs, heart, bones and soft tissue. Chest X-rays are widely available around the world. There could be still some areas where chest X-rays are still not available to the patient population. Chest X-rays are generally quick and easy to perform. They are also easy to learn with a short learning curve. I was able to learn to obtain chest X-rays in an hour while working in a mission hospital. Once you learn the technique and patient positioning, it is generally easy to obtain. It is relatively inexpensive compared to CT scan. It is great for diagnosing obvious or significant pathology.
Unfortunately, X-rays do involve exposing the patient to harmful ionizing radiation. X-rays have been found to be less sensitive to detecting subtle lung pathologies such as a small pleural effusion or early stage of pneumonia, small pneumothorax or increased interstitial fluid. Since ionizing radiation is involved, it is not advisable for serial studies. Chest X-rays will continue to play a role in medicine. But we can adopt a hybrid approach and avoid repeat chest X-rays and perhaps consider follow up with lung ultrasound.
Lung Ultrasound
Lung ultrasound has gained significant traction, especially in emergency and critical care settings. It offers real-time, radiation-free imaging that can be performed repeatedly at the bedside. With the development of commercially available small handheld ultrasound devices, it has made ultrasound highly portable and available virtually anywhere in the world with the least inconvenience and high cost.
Ultrasound provides real-time dynamic imaging and is a highly sensitive imaging modality for detecting pleural effusions and pneumothorax in addition to other lung pathologies. Ultrasound is more operator dependent and cannot be used to view deeper structures in the chest if normal aerated lung is present superficially. It is important to learn the proper techniques and understand the limitations of the device and the technology. Lung ultrasound for the diagnosis of pneumothorax was identified as the #1 POCUS practice domain to be learnt by every POCUS user in the POCUS25 research study published in March 2024.
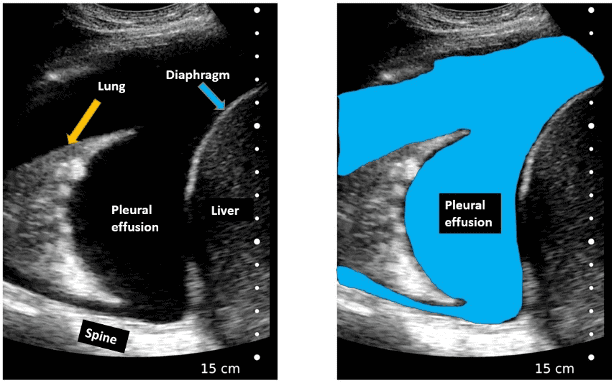
Figure 2. Right side pleural effusion with a positive spine sign. Observe there is atelectasis (collapse) of the right lung. On real time B-mode imaging you will be able to see the atelectatic lung moving within the anechoic pleural effusion resembling a jellyfish (Jellyfish sign). Note that a large pleural effusion like this can be diagnosed on a chest ray effectively. However, posterior-anterior upright chest X-ray may not be sensitive enough to confidently diagnose a pleural effusion less than 200-400 mL or even more depending on patient’s body habitus. Ultrasound can detect free pleural effusion as low as 3-5 mL using correct technique and patient position with an appropriate transducer. Lateral decubitus chest X-ray is more sensitive than a chest PA view and can detect a pleural effusion of more than 50 mL.
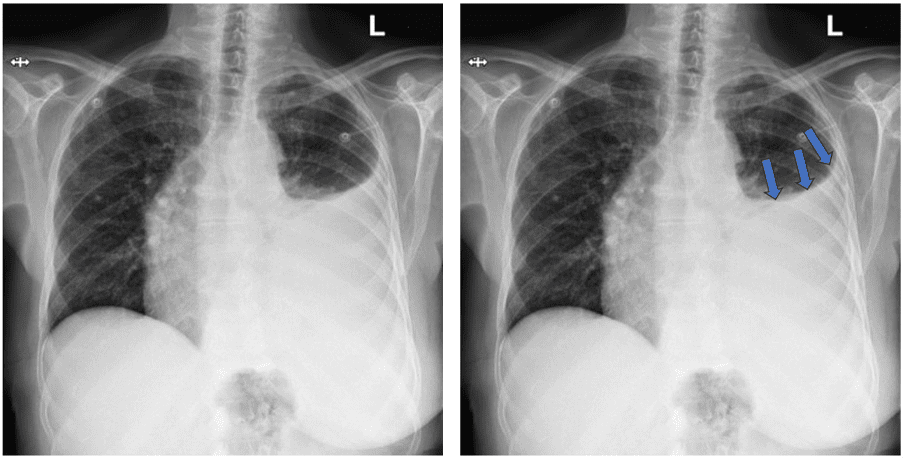
Figure 3. Large left pleural effusion. Observe the concavity of the fluid meniscus (arrows) and the increased distance of aerated left lung from the gastric bubble in the chest X-ray posterior-anterior view (upright). If the X-ray was taken in the supine position, it would not show the fluid meniscus. Instead, an increased haziness would be seen on the affected side. Image courtesy of Radiopedia.org.
Comparing Diagnostic Accuracy
Recent clinical studies have shown that lung ultrasounds often outperform chest X-ray in detecting certain conditions. See a brief comparison below. These numbers may vary slightly in different studies. We can all agree that lung ultrasound seems to be more sensitive the chest X-rays. See the table below.
| Lung/Chest Pathology | Lung US Sensitivity | Chest X-ray Sensitivity |
| Pneumothorax | 92% | 52% |
| Pleural Effusion | 93% | 65% |
| Pulmonary Edema | 97% | 83% |
Table 1. Comparison of sensitivity of lung ultrasound versus Chest X-rays in certain lung or chest pathologies.
Conclusion
While chest X-rays remain valuable, lung ultrasound offers distinct advantages in many clinical scenarios. Its portability, lack of ionizing radiation, and higher sensitivity for certain pathological conditions make it an excellent complementary tool to traditional imaging. As more clinicians become proficient in lung ultrasound, it is likely to play an increasingly important role in respiratory system assessment and management as well as to reduce unnecessary exposure to ionizing radiation, especially in the pediatric age group.
By understanding the strengths and limitations of both modalities, clinicians can choose the most appropriate imaging technique for each patient’s needs, leading to improved diagnostic accuracy and patient care. I feel that chest X-rays will continue to be part of patient assessment in addition to ultrasound. Unnecessary serial chest X-rays could be avoided by the proper use of lung ultrasound when possible. The hope is that there will be global adoption of lung ultrasound leading to increased patient safety.
References