Victor V Rao MBBS, DMRD, RDMS (APCA)
Deep venous thromboembolism (DVT) affects one to two individuals per 1000 each year in the United States. According to the Centers for Disease Control and Prevention, up to 900,000 people could be affected in the US every year. Due to this alarming number, it helps to be aware of the conditions that predispose some to be more prone to developing a DVT.
DVT and pulmonary embolism (PE) are of particular interest as both are preventable in some cases. Early detection and treatment could potentially prevent death. When the thrombus breaks off in the deep veins of the lower extremities, it travels to the right heart. It eventually travels via the pulmonary artery and can cut off the blood supply to the lung or a segment of the lung, resulting in PE. If the clot is large, it can also lead to sudden death, which occurs in up to 25% of patients with PE.
Rudolf Virchow, a physician from Berlin, conducted extensive research on venous thrombosis during the nineteenth century. He proposed that three main factors contribute to the formation of venous thrombosis. These are known as Virchow’s triad and include stasis, intravascular vessel wall damage, and hypercoagulability. This blog discusses May-Thurner syndrome, which could put an individual at high risk of developing a DVT in the left lower extremity.
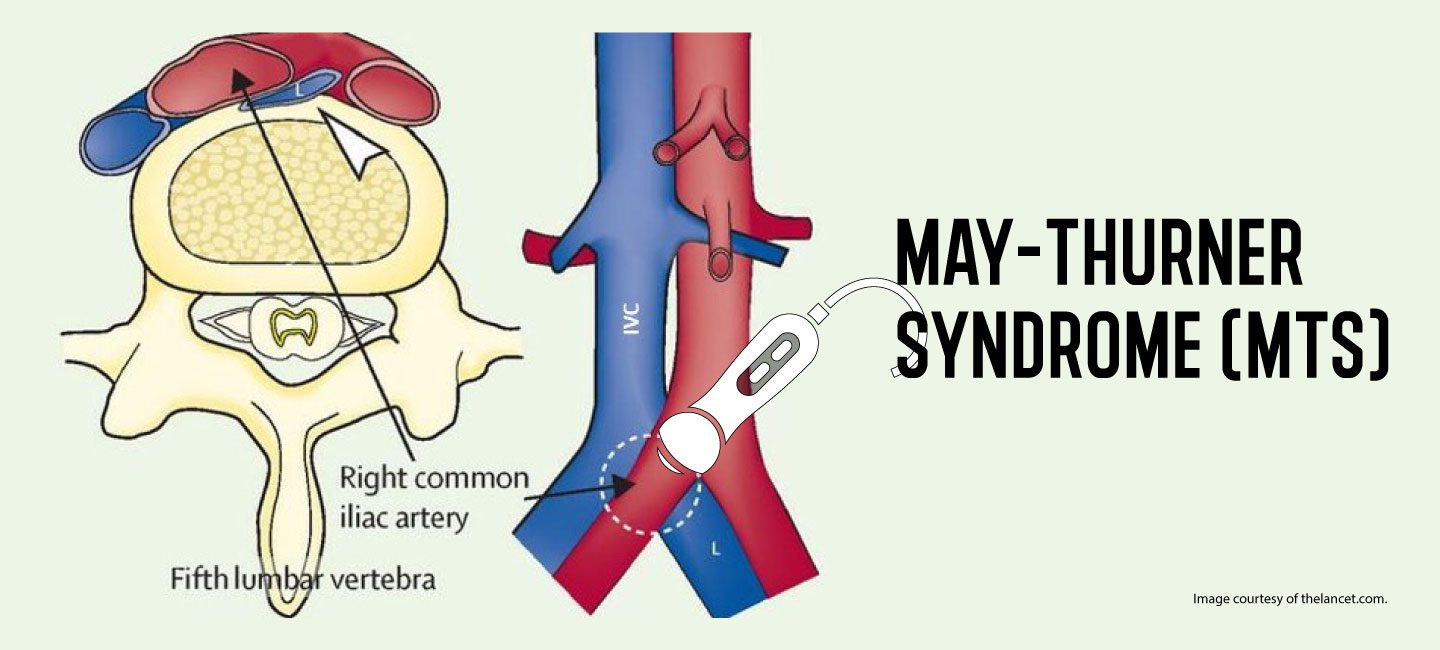
May-Thurner syndrome is also known as left iliac vein compression syndrome and was first defined by May and Thurner in the early 20th century. Cockett further explained the mechanism of action in 1967. It is not a genetic anomaly. It is just a variation in the anatomical relationship of the blood vessels resulting in the compression of the left common iliac vein by the right common iliac artery in the iliocaval region.
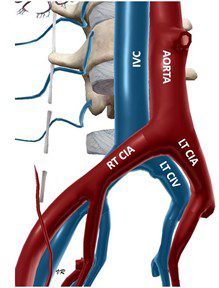
Fig 1. Normal orientation of the right common iliac artery. The right common iliac artery is not running anterior to the left common iliac vein, thus not compressing it. Compare with the figure below.
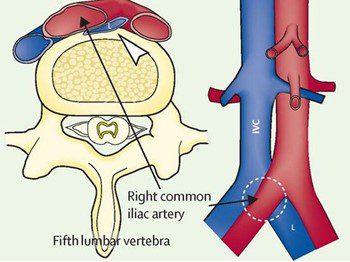
Fig 2. Abnormal orientation in May-Thurner syndrome. The right common iliac artery (RCIA) is seen crossing over the left common iliac vein (LCIV). The cross-sectional image shows the LCIV being compressed between the RCIA and the L5 vertebra. Image courtesy of thelancet.com.
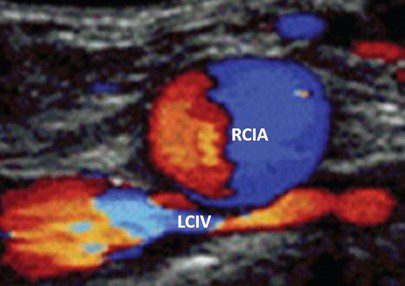
Fig 3. Color Doppler image shows the right common iliac artery (RCIA) crossing anterior to the left common iliac vein (LCIV) and compressing it.
This results in partial venous flow obstruction (stasis) and creates an ideal site for thrombus formation. Individuals with this condition could be asymptomatic or may present with pelvic pain, left lower extremity swelling, and varicose veins in the left leg. In post-thrombotic patients, these individuals may present with chronic leg ulcers, varicose veins, and pigmentation in the left lower extremity.
Initially, in stage 1, there is common iliac vein compression without any structural changes. In stage 2, there is venous spur formation, which presents with edema and or DVT in the left lower extremity. Stage 3 presents as a DVT in the left lower extremity along with edema and some late changes such as varicose veins. Patients with a DVT may benefit from a stent placement in the region of stenosis. However, the DVT may recur on the left lower extremity.

Fig 4. Side by side comparison of lower extremities in a patient with May-Thurner syndrome. Observe that the left lower extremity appears swollen compared to the right side. Image courtesy of AHA Journals.
Treatment options in symptomatic patients include angioplasty with stent placement within the narrowed segment of the vein, bypass surgery, or even repositioning the artery. In conclusion, clinicians should be aware of May-Thurner syndrome. This condition should be ruled out in individuals with a DVT, swelling, or secondary changes in the left lower extremity.
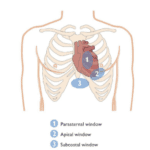
Validate your POCUS skills for deep vein thrombosis with the POCUS Lower Extremity DVT Certificate! Learn more.
About the Author
 Victor V Rao MBBS, DMRD, RDMS (APCA), is a radiologist by training and former director of ultrasound education at University of South Carolina School of Medicine and now works at Inteleos as the Global Clinical Content Manager. Dr. Rao has also worked as a primary care physician in mission hospitals overseas where he enjoyed seeing patients in the clinic, managed inpatients, performed deliveries, C-sections, and minor surgeries.
Victor V Rao MBBS, DMRD, RDMS (APCA), is a radiologist by training and former director of ultrasound education at University of South Carolina School of Medicine and now works at Inteleos as the Global Clinical Content Manager. Dr. Rao has also worked as a primary care physician in mission hospitals overseas where he enjoyed seeing patients in the clinic, managed inpatients, performed deliveries, C-sections, and minor surgeries.