By Victor V Rao MBBS, DMRD, RDMS Ob/Gyn and Abdomen (APCA)
Pneumothorax is the presence of air outside the lung and in the pleural space. The pleural space is the potential space between the parietal and visceral pleura. Normally, there is no air present in the pleural space. The pleural space has a very thin layer of fluid to provide lubrication during breathing. When you scan a patient’s intercostal space with normal aerated lung under it, you can observe lung sliding. Lung sliding is simply visceral pleural sliding against the parietal pleura. It is best observed using a high frequency linear transducer. Pneumothorax may be seen in certain conditions, such as tuberculosis, penetrating chest trauma, asthma, chronic obstructive pulmonary disease, and cystic fibrosis. Be aware that there are many other conditions that can result in secondary spontaneous pneumothorax without any penetrating injury.
The patient may present with shortness of breath, tightness of chest, fatigue, tachycardia, chest pain and even bluish skin coloration if a significant segment of the lung has collapsed. I remember as a new intern on day one, a 28-year-old-male presented with sudden dyspnea. The patient was in distress and had no history of trauma. Breath sounds were absent on the right side. The diagnosis was obvious clinically, but we still ordered a chest X-ray, and it showed absent lung parenchymal markings on the right side. His trachea showed deviation towards the left side. A diagnosis of right sided tension pneumothorax was made, and we proceeded to insert a chest tube. The patient was stable after the chest tube was inserted. See image below of a similar case but tension pneumothorax on the left side.
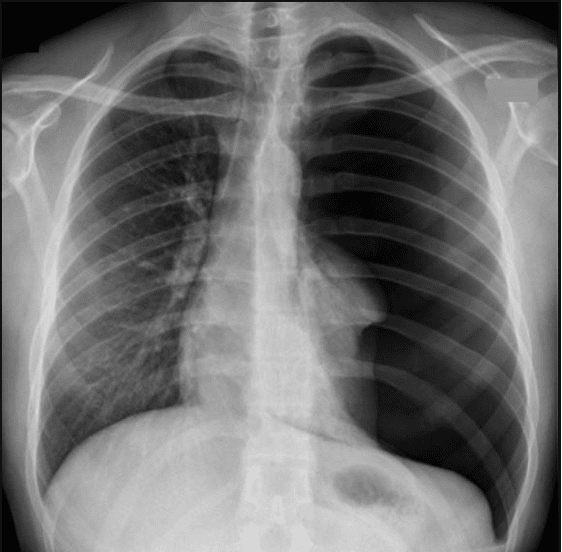
Figure 1. Tension pneumothorax on the left side. Please see reference also. Image courtesy of www.radiologymasterclass.co.uk
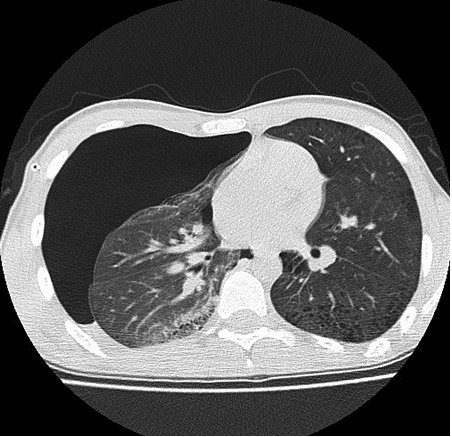
Figure 2. CT Chest shows large right pneumothorax. Image courtesy of BMJ Journals. See reference also.
According to one study chest x-ray had a sensitivity of 52% and a specificity of 100% to identify pneumothorax in trauma patients. Surprisingly, lung ultrasound had a much higher sensitivity of 92% and a specificity of 99.4%. CT scan of the chest had the highest sensitivity and specificity out of all the modalities. The study concluded that lung ultrasound performed by trained users in the emergency department to detect occult pneumothorax was almost as accurate as CT scan.
Both CT scan and X-ray involve ionizing radiation and may take longer to get the results. POCUS lung is a quick and easy modality with a high degree of accuracy without the use of ionizing radiation. Low cost and immediate availability makes lung ultrasound a good modality for detecting pneumothorax.
The ideal transducer would be a low frequency curvilinear transducer. If you wish to just observe lung sliding in detail, you may use a high frequency linear transducer. Be aware that a high frequency transducer may not allow deeper tissue visualization. Some folks also use a low frequency phased array transducer. It depends on what you are comfortable with, and you know what you are looking for.
The patient should be lying flat (do not raise the head end of the bed) in a supine position. Scan the patient’s chest in two locations on both sides of the chest anteriorly. The rationale is that air is light and will rise in the chest cavity if present in the pleural space.
Lung sliding – Make sure the patient is breathing and not holding breath. Lung sliding suggests that there is no evidence of air between the parietal and visceral pleura in the intercostal space region you are imaging with the transducer.
Keep in mind that absent lung sliding can be encountered in a variety of common situations such as:
- Pneumothorax.
- Patient holding breath or not breathing.
- Adhesions – parietal and visceral pleura adhered together.
- Intubation of opposite bronchus only.
A-lines – If there is air in the chest (normal aerated lung) or if there is pneumothorax, you will see A-lines. So, the presence of A-lines only suggests presence of air right under the transducer footprint in that intercostal space. This is not very helpful by itself. It is a reverberation artifact. The “A profile” does suggest no significant fluid/mass in the lung or interstitial tissue in the region of lung tissue and no pleural effusion. See figure below.
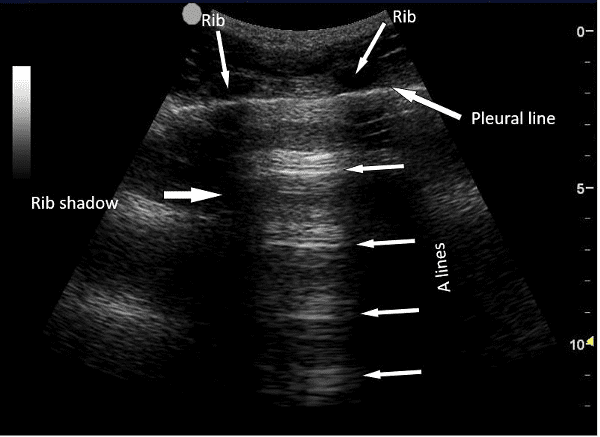
Figure 3. A-lines
B-line – B-lines are very discrete laser beam like reverberation artifact arising from the pleura and they extend all the way into the far field of the lung and move with respiration and unlike A-line they do not fade into the distance. They represent the reflecting interface between interlobular septa and normal lung. Do note that if you see a B-line there cannot be a pneumothorax or air present in the pleural space under the transducer footprint. You may still have to examine other intercostal spaces to do a complete evaluation.
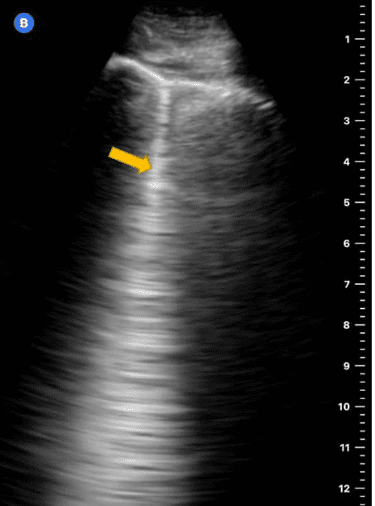
Figure 4. B-line.
Lung Point – Slide transducer more laterally on the chest to localize the lung point. It is a point where the lung sliding ends and pneumothorax begins. It is a very specific sign of pneumothorax. Be aware that you do not confuse it with lung edge. At the bases of the lungs, you will also see the curtain sign as well bilaterally. Please see references for more images and videos.
Seashore Sign
Seashore sign is lung sliding visualized using M-mode. The structures under the transducer footprint all the way up to the pleura appear as bright echogenic horizontal lines. While the normal moving lung during breathing appears grainy or sand like. It is important to make sure the patient is breathing normally and not holding breath.
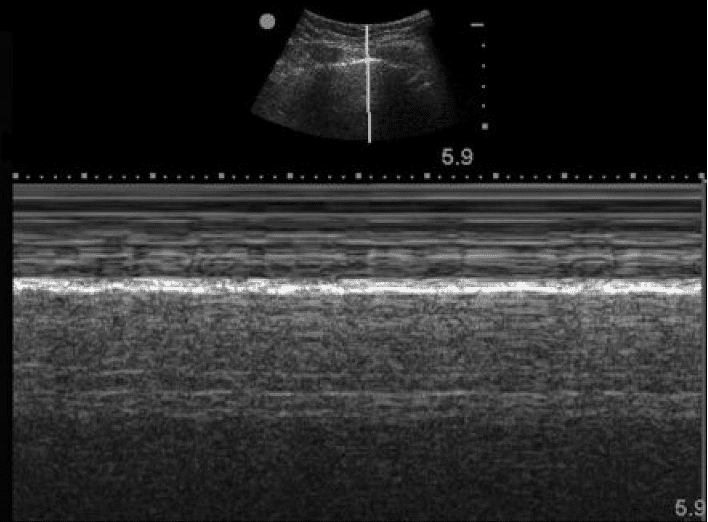
Figure 5. Seashore sign. This is a normal sign and suggest well aerated lung moving normally (lung sliding) with respiration.
Barcode Sign or Stratosphere Sign
The barcode sign obtained when lung sliding is absent. If the patient is not breathing it can create a barcode sign (false positive). The barcode sign suggest the possibility of pneumothorax. See figure below.
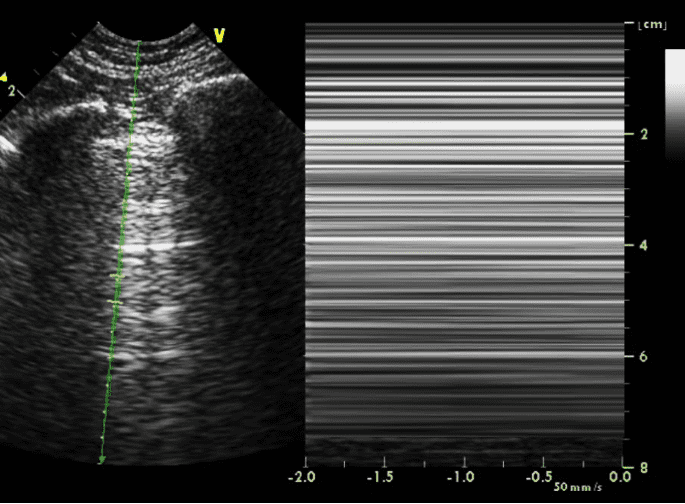
Figure 6. Barcode sign. In pneumothorax.
Conclusion
Lung ultrasound is an excellent modality to evaluate a patient suspected of having occult pneumothorax. You can avoid exposing your patient to unnecessary ionizing radiation. It is a good idea to evaluate the patient before inserting a chest tube to make sure you do not see lung sliding in that intercostal space.
References
https://www.pocus101.com/lung-ultrasound-made-easy-step-by-step-guide/
https://doi.org/10.1378/chest.07-1595
https://www.radiologymasterclass.co.uk/gallery/chest/pneumothorax/pneumothorax_b