01/14/19
Listen to Deborah Crotty, RT (retired), RDMS(AB, NE, OB/GYN), RVT(VT) talk about POCUS, the technology of the future, and how it can create opportunities, not take them away. According to Deborah Crotty, RT (retired), RDMS(AB, NE, OB/GYN), RVT(VT), two-thirds of the world don’t have access to diagnostic imaging and many people are not aware of the advancements of Point-of-Care [Ultrasound]. POCUS can be a game changer and increased awareness is needed.
Looking for additional inspiration? Sign up for our POCUS Post™ newsletter to receive monthly tips and ideas.
Transcription:
James Day: Hello and welcome to the Point-of-Care Ultrasound Certification Academy podcast, where we Focus on POCUS. Here we will discuss all things related to point-of-care ultrasound, the practice, the trends and its impact on health care. Our program will engage thought leaders who are defining global patient care with the stethoscope of the future.
James Day: James Day here today recording live from the Focus on POCUS Studios. Today we have Deborah Crotty as our guest. Deborah was a supervisor in Radiology Interventional Lab and Radiology and Vascular departments and has worked in radiology, vascular and cardiology ultrasound departments in many hospitals. She is our sonographer supreme. She has owned her own ultrasound imaging company for six years, providing cardiology and radiology with billing for ultrasound. Deborah was in clinical applications and was an ultrasound specialist for Phillips and BK [Ana Gaga 00:01:18] corporations, where she also did some work in ultrasound research and development. She has covered a wide geographical region and provided POCUS training and has spent the last seven years doing demonstrations and installations and training for areas such as surgery and emergency departments, ICU units, anesthesia and internal medicine.
James Day: Her training sessions were done in many notable hospitals, mainly Boston Children’s, Harvard Hospital, Cleveland Clinic, John Hopkins and Stanford. Deborah did gel rounds in hospitals with physicians training in areas of POCUS, and has participated in state ACEP emergency educational programs. Also, if that wasn’t enough, Deborah is a contractor for Butterfly IQ and has demoed this new innovative handheld device at American College of Emergency Physicians, ACEP, and the CCM Society of Critical Care Medicine conventions to physicians practicing POCUS. Deborah right now is currently a consultant and independent contractor for point-of-care ultrasound. Deborah, how are you today? Wow, that’s pretty impressive.
Deborah Cotty: Thank you very much. It’s like, get a life. Right?
James Day: I guess you have no time for hobbies or anything else.
Deborah Cotty: I just passed my motorcycle license test, so I’m out there. So I might need point-of-care someday. Who knows.
James Day: God, I hope not. We used to call them murder cycles in the ER. But anyway, I’ll go right to the questions here. For the new healthcare professionals and sonographers who are out there that may be using POCUS in the near future, can you talk a little bit about POCUS?
Deborah Cotty: Absolutely. I first want to say I truly appreciate being invited here today to talk about something I’m passionate about, and I know there are many physicians out there listening that are well versed in point-of-care. But I also know that there are still many that are uncertain about what it is and what it entails. And for me it’s like imagine a world, a medical world, that in less than 15 minutes, not only a doctor but a healthcare provider properly trained, can detect a life threatening condition. And it’s done for a fraction of the cost and in a fraction of the time. Well it’s here, it’s called point-of-care.
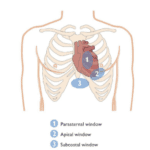
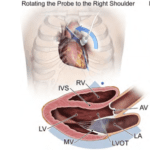
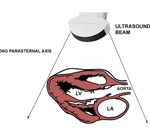
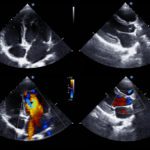
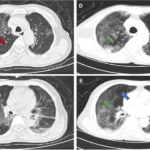
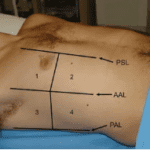
Deborah Cotty: Point-of-care is a limited bedside ultrasound, usually done in 5 to 15 minutes. It’s taking views of the heart, abdomen, pelvis, lungs, some of the vascular studies, and it’s just a qualitative, not quantitative, exam. We just do certain views to get an evaluation, like a triage of the patient. It was originally started in 2004 in Denmark in an ICU department and then it came over to the States. What I see is, unfortunately this technology is developing so much faster than training and certification and many people aren’t aware of the advancements of point-of-care. At the present, point-of-care is the fastest growing area in all ultrasound and it’s been that way for the past 7 or 10 years. It’s growing by leaps and bounds and it’s here to stay. My mission would be to raise awareness of what point-of-care has to offer for everyone.
Deborah Cotty: This new technology can create opportunities, not take them away. And I’m not only talking about sonographers, but cardiologists, radiologists. I’ll tell you, the emergency room was the first to use point-of-care and this happened about 20 years ago. I remember them bringing in a machine, throwing it on the floor and saying, “This is what we’re going to use in the ER because it’s sturdy.” And we laughed at them. We thought, “Look at this monitor and look at this machine. They can’t do what we do.” Well, look who’s laughing now. I think point-of-care at the first stage is at first ridiculed, then violently opposed and then it’s regarded as self evident.
Deborah Cotty: And I’ll tell you, I think the emergency department was a big leader they’ve set the standard for other places in the hospital to follow as far as credentialing and billing. Other areas in the hospitals that are doing this now are ICUs, anesthesia, and now internal medicine is a big one. And there’s going to be other areas throughout the world that are going to be using point-of-care.
James Day: Gosh, I remember with cardiology fellows, I would teach them a basic subcost on a Hewlett Packard 5500 and I had a little preset called the Residents Preset Button. But I was doing it mainly so they wouldn’t beat me over the weekend to come in to do it. And that was the ’90s. Can you give the audience and myself a grand sweep of the future of point-of-care ultrasound. What do you think the future of POCUS is?
Deborah Cotty: Well, the future is going to be dynamic. First of all, what’s interesting, and I had to look this up because I didn’t believe it, healthcare in the U.S. is the fourth largest industry. Isn’t that incredible? And physicians are becoming more and more accountable, healthcare systems are becoming more complicated. In the U.S. we’re spending $10,000 per person, that’s 18% of the GDP, which is the gross domestic product, while two-thirds of the world don’t have access to diagnostic imaging. So it’s out there. It’s going to be used in so many different areas, like in missionary work, military, cruise ships. I remember in the ’70s when the Russians were up in space for a year at a time, when they came back they were taller, thinner, and their muscles had atrophied. So when I worked at Cape Canaveral, ATL put up an ultrasound machine in the shuttle, it was voice activated. And I really wonder if that’s where point-of-care started. And it’s going to be used in ambulances, you could go on and on I think with thinking about it.
Deborah Cotty: First it was initially used by physicians, but now the PA’s are excited about it. Nurses doing dialysis, sonographers, midwives, EMTs, missionary workers. It’s just unprecedented what’s happening with point-of-care in the U.S. Education for doctors now has really escalated in med schools. They did a pilot program at Harvard and they liked it so much that now they’re implementing ultrasound training in med schools and the emergency departments now have fellowships for a year where they learn how to do ultrasounds to contribute to the rest of the department. It’s amazing, I think.
James Day: Yeah, it’s really exploded a lot more. As sonographers, it’s nice knowing that we were there in the beginning. And I remember pushing a giant oven-sized machine down the hall into the units and moving ventilators, and the technology has just shrunk more and more. So regarding technology, Deborah, what about the disruptive aspects with the technology in point-of-care ultrasound?
Deborah Cotty: This is where things get exciting I think in point-of-care. First of all, when I heard disruptive, I go, “That’s a disturbing word.” I said, “Is that good or bad?” I think it’s something the engineers brought up. I’m not quite sure. It’s a big buzzword now, but I would rather think of it as breakthrough, game changer, revolutionary. And the description of a disruptive technology is one that displaces an established technology, shakes up the industry, or a groundbreaking product that creates a completely different industry. I know just recently in the Journal for Critical Ultrasound, they talked about is point-of-care disruptive, formulating why POCUS is different from conventional ultrasound. And it’s interesting to read that. It’s something you can look at.
Deborah Cotty: I think one of the most disruptive things have been these handheld units that came out in 2015. I don’t know if you’re old enough or have seen other repeats of Star Trek. Their Doctor Spock used a tricorder and he went and analyzed what was going on with people and I honestly believe that was the first handheld one. And we talked about it in the future and the future is here. These handheld units are smaller, faster, cheaper, and getting smarter with artificial intelligence. There’s four types out right now. The Butterfly, Phillips has one, GE, and Clarius. And I think this is the real stethoscope or something we’re going to have in our first aid kits in the future. Do you have any questions about that one?
James Day: Well, I just wanted to say that I’m actually a lot older. I’m more of a Lost in Space guy. So I don’t remember the Star Trek. I remember Will Robinson and the robot. That was it.
Deborah Cotty: Okay. The second thing I think is artificial intelligence, which they call AI. And it’s done through deep learning using algorithms. It’s almost the holy grail of diagnostic imaging now. It’s an area of research that has been FDA approved. There’s two companies that do this, one in Israel and the other one called Bay Labs in the U.S. And algorithms are basic building blocks of the computer, and in ultrasound it’s a math equation and flow chart done by tens of thousands of tracings of images, teaching the computer to understand exams or to think like a sonographer. Ejection fractions can be done now just with clips of the heart with two views, and evaluation of the IVC and the outflow track all can be done with AI now. For an end user that’s not really good at doing the heart, this really helps things out.
Deborah Cotty: And also, artificial intelligence can tell you if, the parasternal long is good or bad and how to fix it. In medicine, this technology, it can be more accurate than radiology. Actually, they did a study and had a radiologist define tumors and the computer define tumors. And guess who won? The computer. And is it going to replace the radiologists? Of course not. But it might be a virtual radiologist’s assistant. After all, you can’t sue a computer, right?
James Day: That’s right. And you know something else, I’m glad that AI is doing the ejection fraction because tracing that endocardial border architecture and then trying to do a bullet or a Simpson’s. That was always interesting.
Deborah Cotty: Yeah, and it took time. Or otherwise you did a 3D image and you’d have to do the Simpson’s in two different views. And if you look online under this company, it tells you a lot about this new technology that’s out there. It’s amazing. And it’s going to make it easier for end users to do things that it’s taken us years to learn how to do as sonographers.
James Day: Yeah. And then you talk all about the storage and stuff like that, the iCloud and everything else.
Deborah Cotty: Oh yeah. That’s another thing. Now they have HIPAA compliant apps. They have HIPAA compliant cloud for storage. We have to have EMRs, which are electronic medical records, for not only the patient information, but for images. Another disruptive technology which is kind of old is tele-guidance. And they’ve used this in veterinary medicine a lot. They’ll do a dog and then they’ll send it to a cardiologist or radiologist and have it read. But what they’re doing now, they’re showing the image that you’re scanning, they show the transducer in your hand and a sonographer can tell you how to make the image better. That’s where sonographers come in and help. Or else the reading physician can give the report right then and there. So tele-guidance is being used in these handheld ultrasound machines more and more.
Deborah Cotty: And the fourth thing I want to talk about is chip technology. This is technology that they use in your phone, your computer, and your digital cameras. It replaces the traditional transducers with the peizoelectric crystals, it replaces the ultrasound system, and it’s all done on one single silicon chip that has 9,000 programmable sensors. So it’s unlimited where that’s going to go. It’s affordable and portable and everything is put into the cloud and powered by artificial intelligence.
James Day: That’s amazing.
Deborah Cotty: I know, isn’t it? It’s scary and it’s amazing.
James Day: In our lifetime. So, let’s talk about some down to earth stuff. And so we come down from our sonography cloud, and talk about the billing. What is the status of billing that you’ve seen in your many travels around the country?
Deborah Cotty: Well, I’ll tell you since I billed, this is kind of an interest, especially for me. Once again, the emergency department has really been the department that sets the standard for others to follow. The fellows in the ER had to be credentialed and they do these exams. And what happens in a hospital setting, you have CPT codes and you have diagnostic codes that you have to choose from to be able to get the CPT code paid for by the insurance company. The billing has two components. It has the professional component, which is the doctor that usually is reading, and then it has the technical component, which is who owns the machine. So in a hospital setting, the hospital bills for the technical component and the doctors bill for the professional component.
Deborah Cotty: And the ER has established codes that are done for like FAST exams they order and things like that that they do. Where initially they were doing all these exams and not getting paid for it. It’s going to be interesting. And I think it’s a blue ocean out there really, because when you do an ultrasound scan in an outpatient facility, Medicare, which is really kind of the governing entity when it comes to billing, they kind of govern what the more expensive insurance companies will pay versus Medicaid. But when you have a patient done in an outpatient setting, if you have two ultrasound exams, they’ll pay full price for the first one and half price for the second. Now, when they do this port-of-care billing, they have like a cafeteria style in the hospital and they get paid, sometimes limited, but they get paid for those exams.
Deborah Cotty: So what I am curious to see what happens when point-of-care is done in missionary work, in the military, and these other places outside the hospital setting, are they going to bill? Who’s going to certify them? Are they going to be supervised by a physician so they can be billed like an IDTF, which is a mobile company that is independent from a hospital but they still have supervisors like radiologists and cardiologists to supervise the exams being done. I think it’s going to be real interesting to see where this goes in the next 5 or 10 years.
James Day: Yeah, I’ve got a quick question for you. I’m thinking of, the patient comes in, they get a standard POCUS exam by the physician to answer the question. This is an ER scenario. So that’s a full payment. And then if they recommend a followup done by a sonographer, the full exam, that is paid only half price. Is that right?
Deborah Cotty: No, this is a good question because a lot of times when they’re doing right upper quadrant, left upper quadrant, they’re billed limited. Now if they see something, they’re directed to the radiologist department and they do a full quantitative, a full exam and they’re billing for the full abdomen and they can both get paid. There’s some questions on what goes on. I remember I was in an ICU department one day and I was doing an installation and this cardiologist came up and was really upset about them doing the cardiac exams. And I said, “First of all, at that time we don’t get paid. We’re going to send them to your department for the quantitative, the report package, things like that. We’re just using it as a triage.” And he was rest assured. But that is pretty much what’s happening, and like I said, a lot of stuff is still in the gray area, although the emergency department has really stepped up with this and they’ve been doing it for 15 or 20 years now. But billing is an important area and I’m going to see what happens. It’s going to be interesting, I think.
James Day: One of the things that I’m always wondering what’s going to happen is, if the state, the insurance company mandates a specific certificate or credential before they’ll pay, because I remember at one time when I was a sonographer, I don’t know if it’s still true, but in the lab you only needed one sonographer to be credentialed. And the other ones … Is that still the thing?
Deborah Cotty: Yes. Right now to bill, let’s say with Medicare, either everybody’s registered in maybe echo, or you can have a certified department where one person is registered and they oversee everything in the department that’s certified. Now reading, at least in the state of Michigan, you don’t have to be a cardiologist or radiologist to read an ultrasound. If it’s done in your office you can read it yourself. So it’s interesting what’s going on in billing out there, and like I said, it’s going to be interesting to see what happens in point-of-care because people want to be able to pay for what they have done and what they buy.
James Day: Yeah. I wonder how they’re going to handle that with like, say, an ultrasound-guided procedure. Will that ultrasound be a part of that billing in addition to the actual procedure?
Deborah Cotty: I was reviewing this and I think there is a CPT code for ultrasound guidance of placement of catheter. And they could put a modifier on. Maybe they attempt it and couldn’t do it, that’s when they put those modifiers on the CPT codes.
James Day: Oh, okay. Yeah, that sounds complicated.
Deborah Cotty: Billing in diagnostic imaging is an art. I had to go through three billers before I found someone that I liked. Because you can bill and you can go to school, but diagnostic billing is a different ballgame.
James Day: Right. Right. Wow. Yeah, I guess I’ll get it all ironed out eventually, where it’s moving to. It’s great. You’re actually our first sonographer on our podcast here. I’m glad to have you, Deborah.
Deborah Cotty: Yay. First but not last, right?
James Day: Yes, yes. We’ve got a lot of people on the podcast. Wow. A lot of information, and Deborah, I want to thank you for taking the time to be here on today’s show. And I appreciate the audience for listening, you guys. Don’t forget we’ve got even more POCUS talk. You can follow us on Twitter @POCUSAcademy and on Facebook @POCUSCertAcademy. And Deborah, wow. It was an honor to have you on our podcast today. Thank you.
Deborah Cotty: It’s my pleasure. And everybody, fasten your seat belts with point-of-care.
James Day: All right. You take it easy.
Deborah Cotty: Okay, thanks. Bye. Bye.
James Day: We hope you enjoyed today’s podcast, Focus on POCUS. Be sure to tune in with us next week for more interviews with thought leaders that are on the forefront of global point-of-care ultrasound.
Speaker 3: The thoughts and opinions expressed in this podcast are the views and opinions of the guests and not those of Inteleos. This podcast is for information purposes only.