By Victor V Rao MBBS, DMRD, RDMS (APCA)
In this blog, we briefly discuss the role and limitations of Point-of-care ultrasound (POCUS) in diagnosing acute appendicitis (AA). We will review the normal ultrasound appearance of the appendix and some typical ultrasound findings you may encounter in acute appendicitis.
The appendix is a blind diverticulum that can vary significantly in length. It is also known as vermiform appendix. It derives from the Latin words “vermis’ and “appendere,” meaning “worm-like” and “to hang from,” respectively. As seen in the image below, the appendix arises from the posteromedial surface of the cecum. It is approximately two to three centimeters caudal to the ileocecal valve. Sixty-five to seventy percent of the appendix are retrocecal in position. Twenty-five to thirty percent are pelvic, and there are some uncommon locations as well.
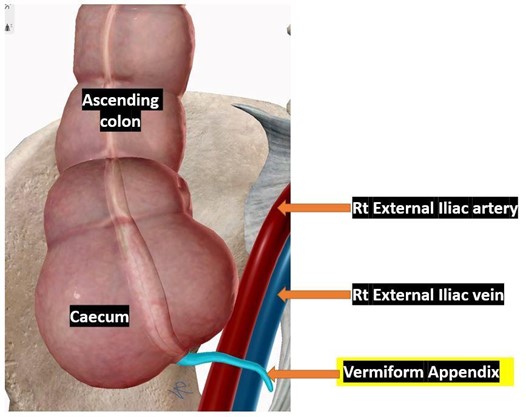
Fig. 1. Vermiform appendix arising from the posteromedial surface of the cecum.
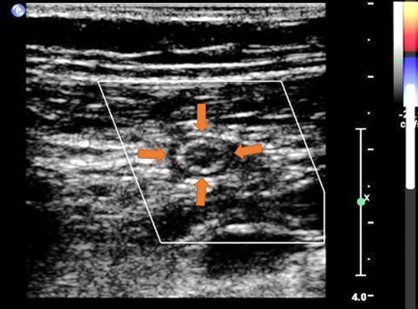
Fig. 2. A normal appendix in transverse view. The diameter is less than six mm. Color Doppler shows no evidence of hypervascularization. Image courtesy of www.radiopedia.org
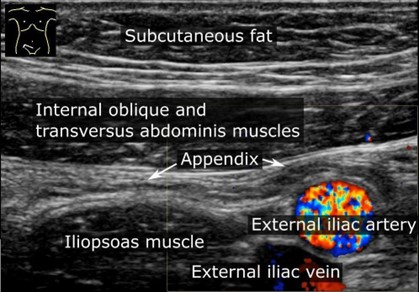
Fig. 3. A normal appendix in a patient suspected to have acute appendicitis. The appendix is not dilated. No appendicolith is seen within the appendix’s lumen, and the diameter is less than six mm. Observe that it is anterior to the iliopsoas muscle and the external iliac artery. Image courtesy of www.wikipedia.org
Approximately 17.7 million cases of acute appendicitis were estimated worldwide in 2019, resulting in over 33,400 deaths. As the term indicates, acute appendicitis is the acute inflammation of the appendix. The patient may present with abdominal pain in the periumbilical region or the McBurney’s point with tenderness in the right lower quadrant, accompanied by nausea, vomiting, and fever. Sometimes the pain could be in an atypical location. Even though a CT scan is very sensitive to diagnose acute appendicitis, ultrasound should be preferred due to its lower cost and absence of ionizing radiation.
Several published studies have concluded varying results about the sensitivity of ultrasound as an effective diagnostic tool for AA. According to one publication by Fabio Pinto et al., the accuracy of ultrasound in the diagnosis of acute appendicitis varies from 44% – 99%, and the specificity range is from 47% – 99%. That is a substantial range in sensitivity and specificity and can be attributed to various factors such as obesity, lack of operator skill, increased bowel gas, and anatomical variants. Despite the challenges, ultrasound should be the first-line diagnostic tool of choice for the reasons mentioned above. Additionally, it is easy to access and available at the bedside.
The ultrasound exam should be performed in the supine position. Recent studies have also recommended additional patient positions if the appendix is not visible in the supine position. The transducer of choice should be a curvilinear low-frequency transducer or even a high-frequency linear transducer in thin subjects or some pediatric patients. In obese patients, you would have to use a low-frequency convex transducer.
Start scanning by placing the transducer over the region of maximum tenderness. The goal should be to identify the appendix. Alternatively, you can begin scanning with the transducer over the area of the mid ascending colon and try to locate the cecum and appendix. Bowel gas may be encountered, and that can be moved out of the field of view by graded compression technique and changing the patient position. Be aware that there may be times when the appendix will not be visualized on ultrasound.
If the appendix is visualized, examine it entirely in the transverse and longitudinal planes. On the ultrasound image, the normal appendix shows five layers. The innermost layer is echogenic and corresponds to the interface of the lumen of the appendix and the mucosa. Next is the hypoechoic mucosa, followed by the hyperechoic submucosa, the darker/hypoechoic muscularis propria. The outermost layer is the serosa, which appears hyperechoic on ultrasound.
Look for the following ultrasound findings that may indicate acute appendicitis.
- Dilated non-compressible appendix
- Maximum appendix diameter of more than six millimeters
- Wall thickness of appendix equal to or more than three millimeters
- Presence of appendicolith within the lumen of the appendix
- Absent peristalsis in the appendix
- Periappendiceal fluid collection or complex heterogeneous collection
- Target sign on transverse view
- Hyperechoic surrounding fat (seen on CT as fat stranding)
- Loss of clear visualization of the appendix wall layers may suggest necrosis
- Defect in the wall of the appendix is consistent with a diagnosis of perforated appendix

Fig. 4. Dilated appendix with a diameter of 1.36 cm or 13.6 mm. The diameter is more than six mm, thus consistent with an acute appendicitis diagnosis. Measure from outer wall to outer wall.
Image courtesy of UltrasoundCases.info, owned by SonoSkills.
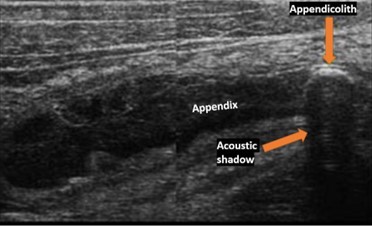
Fig. 5. Acute appendicitis—dilated appendix with an appendicolith. Image courtesy of UltrasoundCases.info, owned by SonoSkills.
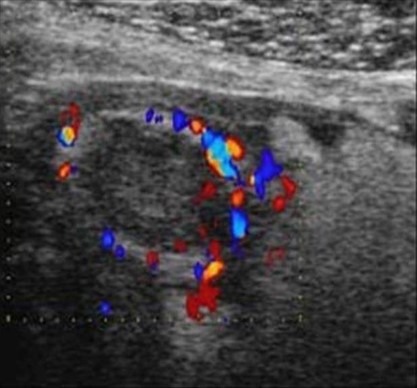
Fig. 6. Hypervascularized inflamed appendix seen in transverse view (Ring of fire on color Doppler). Image courtesy of UltrasoundCases.info, owned by SonoSkills.
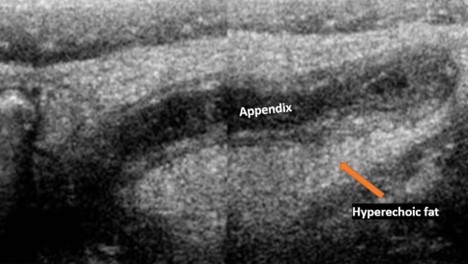
Fig. 7 Appendicitis with hyperechoic surrounding fat. Image courtesy of UltrasoundCases.info owned by SonoSkills.
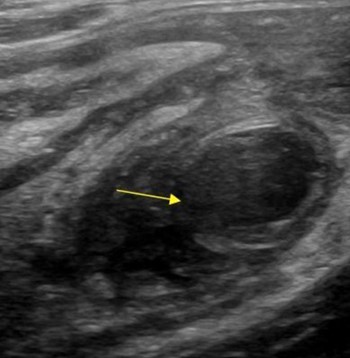
Fig. 8. Perforated appendix with large defect in the wall of the inflamed appendix and a complex collection outside the perforation site. Image courtesy of UltrasoundCases.info, owned by SonoSkills.
In conclusion, POCUS should be the first-line diagnostic tool for evaluating a patient with suspected acute appendicitis. Using sequential positioning may help improve the visualization of the appendix if it is not visible in the supine position. A CT scan should be considered if the appendix is not visualized on ultrasound and there is high clinical suspicion of acute appendicitis or rupture. If there is concern about radiation, an MRI could be considered an alternative.
The hope is that with the democratization and spread of POCUS use worldwide, many will benefit from accurate, low-cost, and timely diagnosis of this potentially life-threatening condition. This may help reduce the mortality due to acute appendicitis and its associated complications globally by aiding with prompt diagnosis and intervention.
References
Park N.H., Oh H.E., Park H.J., Park J.Y. Ultrasonography of normal and abnormal appendix in children. World J Radiology 2011; 3(4): 85-91. Retrieved from https://www.wjgnet.com/1949-8470/full/v3/i4/85.htm
Pinto, F., Pinto, A., Russo, A., Coppolino, F., Bracale, R., Fonio, P., Macarini, L., Giganti, M. Accuracy of ultrasonography in the diagnosis of acute appendicitis in adult patients: review of the literature. The Ultrasound Journal 2013, S2. Retrieved from https://theultrasoundjournal.springeropen.com/articles/10.1186/2036-7902-5-S1-S2
Wickramasinghe, D.P., Xavier, C., Samarasekera, D.N. (2021). The worldwide epidemiology of acute appendicitis: an analysis of the global health data exchange dataset. World Journal of Surgery 2021; 45. Retrieved from https://link.springer.com/article/10.1007/s00268-021-06077-5





















