By Victor V Rao MBBS, DMRD, RDMS
The long head of the biceps tendon (LHBT) is a common source of anterior shoulder pain. Musculoskeletal Point-of-Care Ultrasound is an excellent modality for evaluating the LHBT and diagnosing common pathologies affecting it. In this blog article we will delve deeper into this topic and refresh the relevant anatomical details of this structure as well learn how to examine LHBT using POCUS and look at normal sonographic findings as well as learn to recognize ultrasound findings in common pathology affecting this structure.
The goal is to familiarize POCUS users with the characteristic findings of some of these conditions so you can make the correct diagnosis confidently. Do note that some images and some graphics may not be an exact representation, and some ultrasound images may not be very clear. I have attempted to make it as clear as possible and added some useful references for your review.
Anatomy and Scanning Technique
The LHBT originates from the supraglenoid tubercle of the scapula and the superior glenoid labrum. It courses through the rotator interval and bicipital groove before joining the short head to form the biceps muscle belly.

Figure 1. Long and short head of the biceps brachii seen joining together to form the biceps muscle belly. See figure 2 also.
It passes obliquely through the shoulder joint, enclosed in a synovial sheath. It exits the joint and enters the bicipital groove (intertubercular sulcus) of the humerus. It descends the groove, still enclosed in its synovial sheath. It exits the distal end of the groove and joins with the short head of biceps tendon. The intra-articular portion of the tendon is flattened and slightly larger in cross-section. It transitions to a more rounded, smaller cross-section as it enters the bicipital groove. The tendon is approximately 9-10 cm long and 5-6 mm in diameter.

Figure 2. Long head of the biceps brachii muscle and tendon highlighted in blue. In this blog article we will only be looking at the LHBT tendon in detail.


Figure 3. Close up view of the long of the biceps brachii with the articular capsule removed. The articular capsule is highlighted in the image on the right.
Functions of LHBT
The long head of the biceps tendon has some mechanical functions. They are:
- It acts as a weak flexor of the shoulder joint.
- It also acts as an abductor of the shoulder joint.
- It helps to stabilize the humeral head.
- It helps flex the elbow joint in conjunction with the short head of biceps.
- It assists with supination of the forearm.
Common Pathology of LHBT that can be Diagnosed with MSK POCUS
The LHBT can commonly undergo degeneration due to mechanical stress or be injured. We will look at some common conditions that we may encounter in the POCUS setting.
Procedure
To examine the LHBT, the patient should be seated with the arm in neutral position, elbow flexed to 90°, and forearm supinated. The transducer is placed transversely over the anterior shoulder to identify the bicipital groove between the greater and lesser tuberosities.
Figure 4. Probe position for imaging the long head of biceps tendon in the bicipital groove. Note that the probe marker is pointing towards the patient’s right side. Some groups use a different orientation protocol and have the probe marker point towards the midline of the patient.
Transverse view of LHBT
The tendon appears as an oval or slightly round hyperechoic structure within the bicipital groove. The tendon should be centered within the groove and measure approximately 5-6 mm in anteroposterior diameter. The length of the tendon is approximately 9.0 cm. Scanning proximally allows visualization of the tendon entering the glenohumeral joint. A longitudinal view is obtained by rotating the probe 90 degrees with the LHBT tendon in the middle of the screen.
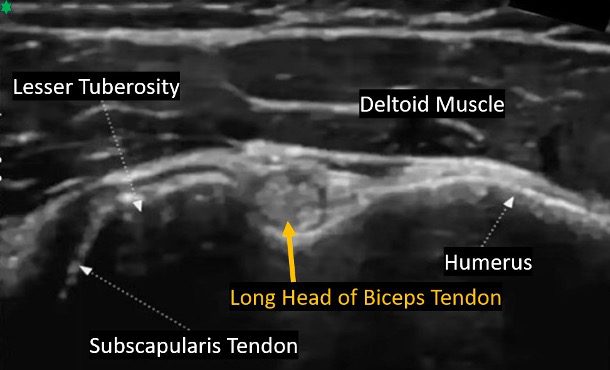
Figure 5. Transverse view of the long head of the biceps tendon in the bicipital groove.
Longitudinal View of LHBT
A longitudinal view is obtained by rotating the probe 90 degrees when an optimal transverse view of the LHBT has been obtained. In a longitudinal view, the fibrillar pattern of the tendon fibers should be visible clearly. A thin hypoechoic rim of fluid in the tendon sheath is a normal sonographic finding. As you slide the transducer down towards the elbow you will be able to observe the tendon continuing as the biceps brachii muscle.

Figure 6. Probe positioning for the longitudinal view of the long head of the biceps tendon. Note that the probe orientation marker is pointing cephalad (towards the patient’s head).
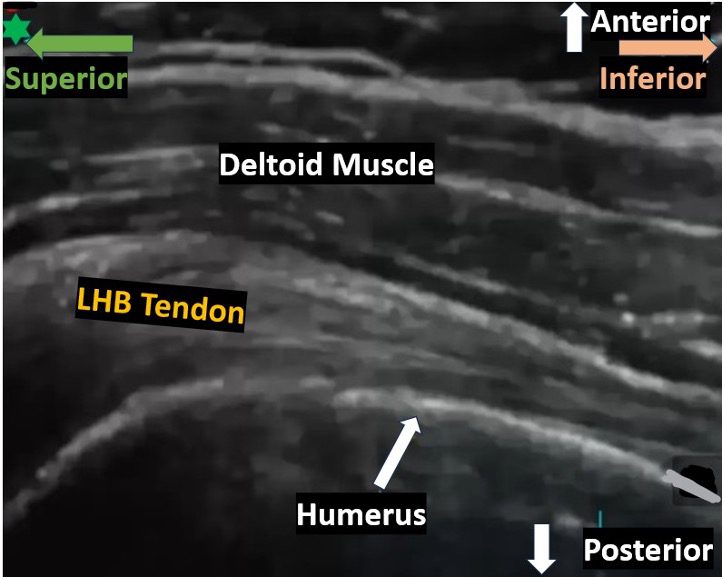
Figure 7. Longitudinal view of the long head of the biceps tendon. These are normal findings.
Common Pathological Findings on POCUS of the LHBT
Some common pathologic findings on ultrasound include the following.
| Pathology | Ultrasound Finding |
| Tendinosis | Tendon thickening >4 mm with heterogeneous echotexture. |
| Tenosynovitis | Hypoechoic fluid surrounding the tendon, often with synovial hypertrophy. |
| Partial-thickness tear | Focal hypoechoic or anechoic defect within the tendon. |
| Full-thickness tear | Complete disruption of tendon fibers with retraction and anechoic space/blood in the space in between the two ends. |
| Subluxation | Tendon displaced medially and or partially out of the bicipital groove. |
| Dislocation | Tendon completely displaced out of the bicipital groove with an empty bicipital groove. |
Table 1. List of common pathologies of LHBT that can be diagnosed with ultrasound and associated diagnostic ultrasound findings. Please note that there is some variability in literature in the numbers quoted. Please refer to your team guidelines.
Tendinosis
Tendinosis of the LHBT is associated with deep aching pain in the front of the affected shoulder. The patient will experience worsening pain when lifting the arm over the head. The pain may be worse at night and may also radiate to the arm, chest and elbow. The LHBT will show areas of decreased echogenicity and will appear hypoechoic areas within the normal hyperechoic tendon. The hypoechoic areas can be focal or diffuse depending on the severity of the condition. The LHBT tendon may also appear thickened. The normal LHBT transverse diameter in adult females and males is <4.6 mm and <5.5 mm respectively. The tendon transverse diameter can increase up to 9 mm in severe cases.
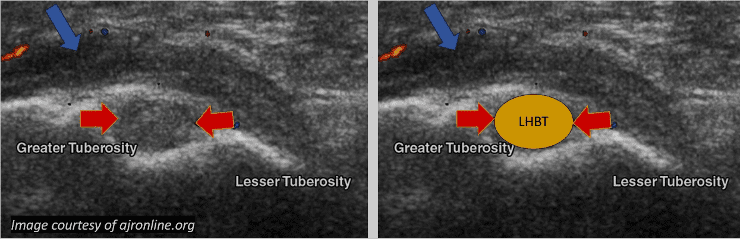
Figure 8. Transverse view shows a hypoechoic and enlarged LHBT (red arrows) consistent with tendinosis. Color Doppler does not show evidence of increased vascularity. Minimal flow seen. There is slight surrounding hypoechoic tenosynovitis. Note adjacent hypoechoic distention of subacromial-subdeltoid bursa.
Ultrasound findings can help grade the severity of the condition as follows.
| Grade | Ultrasound Finding |
| 0 | Normal findings of biceps tendon and tendon sheath. |
| 1 | Only mild filling of the tendon sheath – anechoic ring around the tendon < 2mm. |
| 2 | Anechoic ring around the tendon – tendon sheath 2-3 mm and mildly inhomogeneous tendon. |
| 3 | Tendon sheath is obviously anechoic and markedly widened. |
Table 2. Ultrasound grading of tendinosis.
Tenosynovitis
Ultrasound can effectively diagnose this condition in the LHBT. Diagnostic findings will be tendon sheath thickening, increased vascularity in the tendon sheath that can be documented using color Doppler or power Doppler as well as anechoic or hypoechoic zone surrounding the LHBT as seen in the image below.
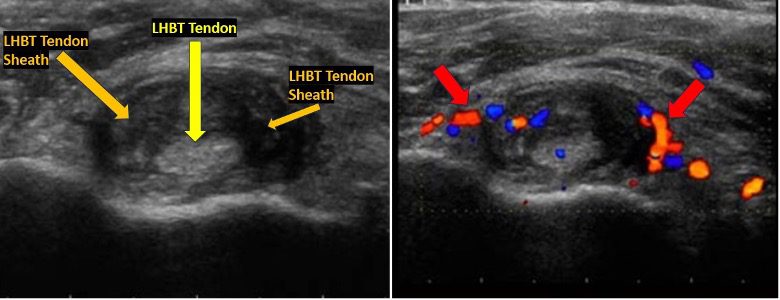
Figure 9. A case of tenosynovitis involving the long head of biceps tendon. Observe the inhomogeneous tendon and the thickened tendon sheath. The color Doppler image on the right shows evidence of increased vascularity due to inflammation. You may also use power Doppler if available to demonstrate enhanced blood flow in the affected region.
Partial-thickness Tear
Partial-thickness tears may be slightly difficult to diagnose using POCUS. Ultrasound findings may show an area of focal thinning of the LHBT or focal loss of the normal fibrillar pattern. There could be anechoic or hypoechoic areas within the tendon. Make sure they are not anisotropy artifact by aligning the transducer perpendicular to the tendon fibers. Ultrasound sensitivity could vary widely from 27% to 71%. Compare findings with the normal side of the same patient.
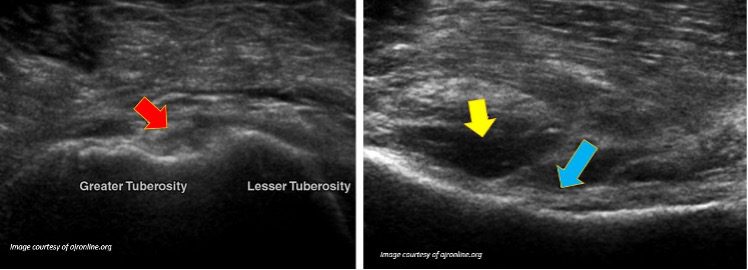
Figure 10. The image on the left shows a transverse view of LHBT. The tendon appears as thin linear tissues which are separated by anechoic areas (red arrow) suggesting partially torn LHBT. The blue arrow is pointing to heterogeneous LHBT tendon with some anechoic areas within it. The yellow arrow is pointing to tenosynovitis adjacent to the LHBT tendon.
Full-thickness Tear
POCUS has a high sensitivity (88% to 100%) to diagnose this condition. Look for evidence of tendon discontinuity and retraction of the torn end of the LHBT. The void region is full of anechoic fluid (blood). You may also perform a dynamic examination to confirm the diagnosis.
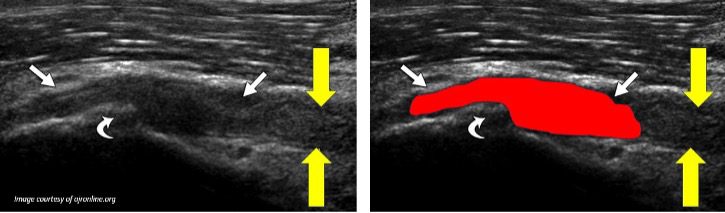
Figure 11. LHBT full thickness tear with an anechoic space in between representing blood. (white arrows). The yellow arrows are pointing to the retracted LHBT. The curved white arrow is pointing to an incidental finding (bone spur). The red highlighted area may be slightly more that the actual blood clot size (diagrammatic representation only).
Subluxation
POCUS has a high sensitivity (96% to 100%) in diagnosing this condition. The LHBT tendon could be displaced medially or laterally to the bicipital groove. Hyperechoic LHBT tendon extending partially beyond an imaginary line drawn from the greater to the lesser tuberosity. Perform a dynamic examination to document the tendon movement and stability.
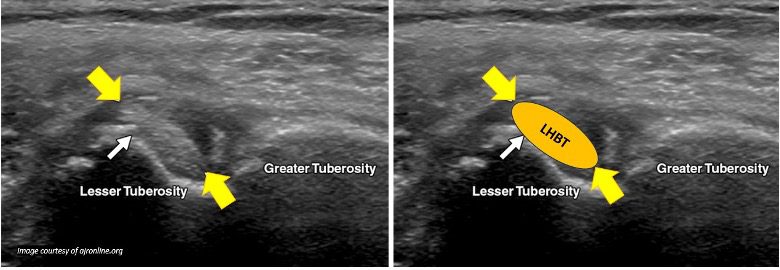
Figure 12. Short-axis ultrasound image of the LHBT shows medial subluxation of LHBT (yellow arrow) with adjacent heterogeneous tenosynovitis. A small white arrow is pointing to a bony spur.
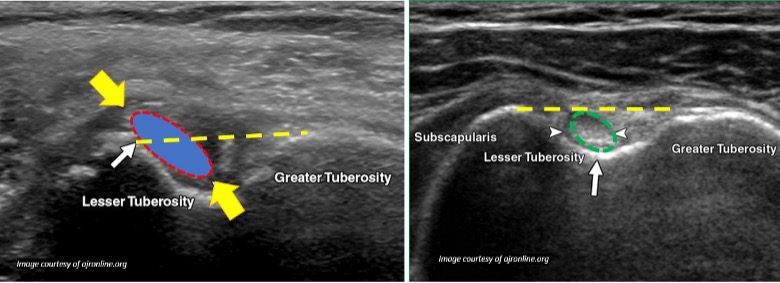
Figure 13. Comparing subluxation of LHBT (left) versus normal LHBT on the right. Observe the yellow dotted imaginary line from the greater to the lesser tuberosity. The LHBT is not only enlarged but also pushed medially in the bicipital groove and is extending beyond the yellow dotted line. It is still seen partially inside the bicipital groove. So, it is a case of subluxation of LHBT. The normal LHBT lies centrally inside the bicipital groove.
Dislocation
Ultrasound offers real-time, dynamic imaging and assessment of the LHBT position and movement within the bicipital grove. In subluxation, the LHBT is partially displaced. In dislocation, the LHBT is completely outside the bicipital groove and the bicipital groove will be empty on ultrasound imaging.
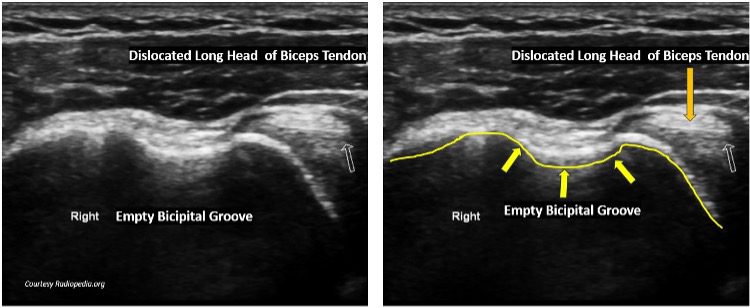
Figure 14. Medial dislocation of the LHBT. The LHBT is seen outside the bicipital groove. The bicipital groove is empty. Compare with the case of subluxation above.
Diagnostic Accuracy of Some Common LHBT Pathology on Ultrasound
Ultrasound has shown high diagnostic accuracy for LHBT as shown in the table below.
| Pathology | Sensitivity | Specificity |
| Full-thickness tears | 88% to 100% | 98% |
| Subluxation/Dislocation | 96% to 100% | 100% |
| Dislocation | 96% to 100% | 100% |
| Tendinosis | 65% to 68% | 70% to 98% |
| Partial-thickness tears | 27% to 71% | 71% to 100% |
Table 3. Sensitivity and specificity of POCUS in diagnosing some common pathologies of the long head of biceps tendon (LHBT).
Final Thoughts
Musculoskeletal ultrasound is accurate, cost-effective imaging modality. It also allows dynamic imaging and evaluation of the LHBT. With proper technique, it allows confident diagnosis of various long head of biceps tendon pathologies to guide appropriate and timely clinical management. Be aware of the anisotropy artifact and practice ways to eliminate that ultrasound imaging artifact to avoid making a false positive diagnosis. Always compare with the normal side and correlate clinically.
References




















