By Hector Lopez-Cardona, MD
Introduction
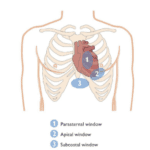
Considering the technological advances in today’s healthcare systems, an important aspect in delivering patient care is to be able to provide holistic and personalized clinical care. Point-of-Care Ultrasound (POCUS) offers the possibility of comprehensive assessment and a bedside insight into treatment response with emphasis on patient safety and quality of care.
In this post, I will discuss reasons why POCUS should be part of modern medicine, its role in delivering personalized care, and aspects that make it a valuable tool for all health professionals.
Why Personalization Matters
The 21st Century Healthcare system requires that clinicians deliver fast paced, and personalized patient care with a high degree of accuracy. POCUS is a great diagnostic and procedural tool that improves the ability to tailor medical interventions in accordance with patients’ needs. The real-time nature of POCUS is appealing because it expedites the clinical decision-making process. To understand why this matters, we can briefly use the VExUS (Venous Excess Ultrasound) protocol as an example of this personalization and how this can make a difference.
VExUS utilizes ultrasound to do an assessment of the fluid dynamics of multiple venous structures like the inferior vena cava, hepatic veins, portal veins, and renal veins. By assessing these different structures, clinicians can accurately determine the degree of venous congestion in each patient as these respond to fluid resuscitation avoiding fluid overload. This comprehensive, individualized assessment allows for an accurate assessment of a patient’s fluid status as it is being corrected, and it is often necessary to construct a personalized treatment plan to improve the outcome in sick patients.
How POCUS Provides Personalized Patient Care
Personalized care is based on medical treatment that is adapted to individual patient characteristics. POCUS supports personalized care by:
- Establishing Trust: POCUS offers the opportunity to establish trust with patients. As a bedside tool, it allows for more productive interactions, building trust and enhancing patient satisfaction.
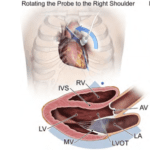
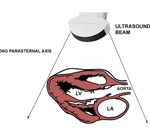
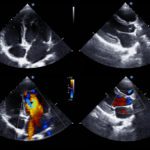
- Quick Identification of Issues as these manifest in individual patients: Immediate visualization of internal structures helps clinicians to diagnose structural and functional abnormalities. For example, in a patient presenting with shortness of breath, POCUS can quickly help to differentiate between cardiac and pulmonary causes, leading to faster and more accurate treatment.
- Allowing a Tailored Treatment Plan: Real-time understanding of the patient’s physiological changes, allows clinicians to individualize treatment plans based on current findings. This personalized approach optimizes interventions that are adequate and effective for each patient in a specific clinical context.
- Quick Adjustments: POCUS offers the possibility of quick reassessment and adjustments of any treatment plan. This ensures that the plan is in accordance with the patient’s needs.
- Avoiding Unnecessary Procedures: POCUS avoids patient’s exposure to unnecessary interventions (e.g.: excessive diuretic manipulation without clear indications, additional imaging studies etc.) by providing an immediate “replay” at the bedside; this is cost effective and avoids potential harm to the patient.
Why is POCUS Essential for Healthcare Providers?
POCUS training is essential for those health professionals who want to provide personalized patient care. I will explain why:
- Improved Clinical Skills: POCUS skills improve the clinician’s diagnostic capability, leading to more accurate and less invasive patient evaluation. While a physical exam provides essential information through observation, palpation, percussion, and auscultation, POCUS adds a layer of precision and immediacy that can significantly enhance patient care. For example, during physical examination of a patient with dyspnea, crackles are heard. At this point a differential must be made and it is here where POCUS can be used as a confirmatory tool to distinguish between COPD exacerbation and congestive heart failure. This is especially relevant in those situations where time is critical, such as the emergency department and critical care units.
- Better Decision-Making: Having real-time patient data allows healthcare providers to make faster and better-informed decisions. Whether you’re dealing with a trauma patient in the emergency department or managing chronic conditions in an outpatient clinic, POCUS gives you the insights you need to choose the best course of action in specific situations.
- Guiding Expedited Interventions: In cases of trauma, POCUS can rapidly detect internal bleeding in both stable and unstable patients but been capable of identifying free peritoneal fluid in a patient with unstable vital signs is crucial as an expedited surgical intervention can be provided.
- Optimized Patient Outcomes: There is literature demonstrating improved patient outcomes when POCUS is applied. POCUS allows early diagnosis and intervention, minimizing complications and enhancing patient safety and quality of care.
Final Thoughts
In conclusion, POCUS is a tool that enhances the ability to provide a comprehensive, real-time assessment of the structure and function of multiple body systems, allowing for an integrated, holistic, and personalized patient care. POCUS ensures that healthcare providers can make well-informed decisions that consider the whole patient.
References
- Whitson, M. R., & Mayo, P. H. (2016). “Ultrasound in the ICU: Applications of Ultrasound in Critical Care.” Critical Care Medicine, 44(6), 1176-1180.
- Narula, J., Chandrashekhar, Y., & Braunwald, E. (2018). “Time to Add a Fifth Pillar to Bedside Physical Examination: Inspection, Palpation, Percussion, Auscultation, and Insonation.” JAMA Cardiology, 3(4), 346-350.
- Levitov, A. B., Frankel, H. L., & Blaivas, M. (2015). “Critical Care Ultrasonography.” McGraw-Hill Education.
- Russell, F. M., Zakeri, B., Amini, R., & Adhikari, S. (2017). “The effect of a point-of-care ultrasound protocol on the clinical management of ambulatory patients with suspected renal colic in a resource-limited setting.” Journal of Emergency Medicine, 52(1), 16-24.